Summary
- A year ago, when the COVID-19 pandemic hit most of the world, there was arguably a good case for lockdowns. The initial growth of the epidemic implied a high basic reproduction number, which in turn meant that unless transmission was reduced the virus would quickly sweep through most of the population because incidence would continue to grow exponentially until the herd immunity threshold was reached, overwhelming hospitals and resulting in the deaths of millions of people in a few weeks. Lockdowns and other stringent restrictions seemed like a plausible way of reducing transmission to “flatten the curve” and prevent that scenario from materializing.
- Many people continue to reason along those lines, but since then we have learned that, whatever the precise effect that lockdowns and other stringent restrictions have, it is not so large that it can easily be picked up in the data, as it would surely be if restrictions had the very large effect that pro-lockdown advocates claim. In particular, it is not the case that the alternative to lockdowns is herd immunity (at least in the short run), because in practice incidence never grows exponentially for very long even in the absence of stringent restrictions. While it is plausible that, without stringent restrictions, incidence would start falling a bit sooner and faster, the data show very clearly that it always starts falling long before the herd immunity threshold is reached with or without a lockdown.
- Many factors likely contribute, but the main explanation of that fact is probably that, despite what simple epidemiological models assume, people modify their behavior in response to changes in epidemic conditions such as rising hospitalizations and deaths, which reduces transmission and causes the epidemic to recede long before the herd immunity threshold is reached. However, until enough people have acquired immunity through natural infection or vaccination, this is only temporary and eventually incidence starts growing again because people go back to more regular behavior. Lockdowns and other stringent restrictions do not have a very large effect because they are a blunt instrument and have a hard time targeting the behaviors that contribute most to transmission.
- The belief that lockdowns are very effective nevertheless persists because authorities react to the same changes in epidemic conditions as the population, so they tend to implement lockdowns and other stringent restrictions around the time when people start modifying their behavior. This means that the effect of voluntary behavioral changes is attributed to lockdowns even if the epidemic would have started to recede in the absence of stringent restrictions. We know this because that is exactly what happened in places where the authorities did not put in place such restrictions, which are extremely diverse economically, culturally and geographically and therefore unlikely to share some characteristics that allow them to reduce transmission without a lockdown.
- Places where the virus seems to have spread more are those where the population is relatively young, which is exactly what the theory presented here–that voluntary behavioral changes in response to changes in epidemic conditions are the main driver of the epidemic–predicts, since a younger population implies a lower rate of hospitalization and death, which in turn means that the virus will have time to spread more before the rise in hospitalizations and deaths scare people into changing their behavior enough to push the reproduction number below 1.
- The scientific literature on the effect of restrictions on transmission contains many inconsistent results, but more importantly it is methodologically weak and therefore completely unreliable. To be sure, many studies found that restrictions had a very large effect on transmission, which pro-lockdown advocates like to cite. However, those results do not pass a basic smell test since one just has to eyeball a few graphs to convince oneself the studies they come from perform terribly out of sample, which is not surprising since most of them either assume that voluntary behavior has no effect whatsoever on transmission or do not use methods that can establish causality by disentangling the effect of restrictions from that of voluntary behavior changes.
- Even if you make completely implausible assumptions about the effect of restrictions on transmission, and ignore all their costs except their immediate effect on people’s well-being, they do not pass a cost-benefit test. For instance, in the case of Sweden (where incidence is growing again and the government is considering tightening restrictions), if you assume that a lockdown would save 5,000 lives (which is approximately the total number of deaths during the first wave, when the population was behaviorally naive and vaccination was not under way), a 2-month lockdown followed by a gradual reopening over the next 2 months would have to reduce people’s well-being by at most ~1.1% on average over the next 4 months in order to pass a cost-benefit. In other words, for a lockdown to pass a cost-benefit test under those assumptions, you would have to assume that on average people in Sweden would not be willing to sacrifice more than ~32 hours in the next 4 months to continue to live the semi-normal life they currently enjoy instead of being locked down.
- While I use Sweden to illustrate my point because it has been a focal point of the debate about restrictions, this exercise yields a similar conclusion almost everywhere else. The truth is that, from a cost-benefit perspective, Sweden’s much-decried strategy has been vastly superior to what most Western countries have done and it is not even close. Even if you think that it would have been better for Europe and the US to follow Australia and New Zealand’s example by adopting a so-called “zero COVID” strategy after the first wave, which would probably not have succeeded anyway even back then, this boat has already sailed and trying to pull it off now makes absolutely no sense from a cost-benefit perspective. Despite popular but confused arguments to the contrary, which I discuss at the end of this essay, this remains true even if you take into account the threat posed by new variants of SARS-CoV-2.
Almost every country in the world has now gone through 2 or 3 waves of the COVID-19 pandemic and, in most of them, incidence remains high although it has recently been falling almost everywhere. everywhere. Although the vaccine is being rolled out in many places, it is at a very slow pace with most countries facing shortage and distribution problems. This means another flare-up is likely in many places even if the worst of the pandemic is probably behind us. While lockdowns and other stringent restrictions had high levels of support when the first wave hit, this is no longer true and, as we are entering the last phase of the pandemic, the debate about how to deal with it has never been so intense. Sweden went a different route last spring by foregoing a lockdown and, while it remains widely vilified for this decision, even some people who thought it was a mistake at the time have changed their mind and now think other countries should follow Sweden’s example and seek to contain the epidemic without stringent restrictions such as stay-at-home orders, outright business closures, etc.
I’m one of them. Back in spring, I was in favor of lockdowns, but since then I have reached the conclusion that lockdowns and other stringent restrictions do not make sense from a cost-benefit perspective. I now think that, even with the information we had at the time, supporting lockdowns was the wrong call because even though I insisted that it was only a temporary solution and that we should be ready to revise our view as more evidence came in, I should have known that people would not and that lockdowns would quickly become institutionalized. However, in this post, I will not be arguing for this view. I only want to argue that, regardless of what should have been done last spring, the data we have accumulated since then show very clearly that, whatever the precise effect of lockdowns and other stringent restrictions, it is not nearly as large as we might have thought, so their costs far outweigh their benefits and we therefore should avoid them where they are not currently in place and start lifting them immediately where they are.
Back in March, there was at least a case in favor of lockdowns. Indeed, we didn’t know at the time how difficult it would be to reduce transmission, but we knew that had been measured at ~2.5 and that in most countries thousands of people were already infected, which meant that unless transmission was reduced quickly more than 90% of the population might be infected in a few weeks. Since the evidence suggested that the infection fatality rate (IFR) was around 1% even when people received proper treatment, this in turn meant that in a country like the United States, between 2 and 3 million people would die even if hospitals were not overwhelmed. However, if the virus swept through the majority of the population in a few weeks, the hospitals undoubtedly would be, so most people would not receive proper care, the IFR would consequently rise way above 1% and the number of deaths would actually be much higher. A lockdown would cut transmission and, while it could not prevent a large part of the population from getting infected eventually, because we couldn’t stay locked down forever, it would “flatten the curve” and prevent hospitals from being overwhelmed and the rise of the IFR this would cause.
But while this line of thought was reasonable at the time, it has become clear that it rested on a flawed premise. Even without a lockdown and stringent restrictions, incidence always starts falling long before the herd immunity threshold is reached. In fact, not only are lockdowns and other stringent restrictions unnecessary to prevent the virus from ripping through most of the population in a few weeks, but they don’t seem to be making a huge difference on transmission. This makes a more liberal approach, not unlike what Sweden has done, far more appealing from a cost-benefit perspective and should have radically altered the policy debate. Unfortunately, this has largely not happened, because most people still believe the flawed assumptions of the original argument for lockdowns and have kept moving the goalposts. At any rate, this is the case I will make in this post.
The alternative to lockdowns and other stringent restrictions is not herd immunity
The first thing everyone should acknowledge at this point, although many people still don’t, is that whatever the precise effect of lockdowns and other stringent restrictions is, it can’t be huge. In particular, it’s certainly not the case that, in the absence of a lockdown, the virus quickly sweeps through the population until the epidemic reaches saturation. There is no need for anything fancy to convince yourself of that, you just have to eyeball a few graphs. Here is my favorite: As you can see, Sweden was ahead of the rest of the EU after the first wave, but the rest of the EU has caught up since then and now the number of COVID-19 deaths per capita in Sweden is about average.
As you can see, Sweden was ahead of the rest of the EU after the first wave, but the rest of the EU has caught up since then and now the number of COVID-19 deaths per capita in Sweden is about average.
Of course, policy is not the only factor affecting the epidemic (that’s the point), so this graph does not show that lockdowns and other stringent restrictions have no effect, but if policy mattered as much as pro-lockdown advocates claim, it would look completely different. Indeed, although Sweden has tightened restrictions to fight the epidemic in recent months and the other EU countries have on the contrary used less stringent restrictions during the second/third wave, restrictions in Sweden remain much less stringent than almost everywhere else in Europe and this was already true during the first wave. In particular, even if they have to close earlier and respect stricter health regulations, bars and restaurants are still open and there is no curfew. If lockdowns and other stringent restrictions were really the only way to prevent the virus from quickly sweeping through the population until saturation is reached, the number of deaths per capita in Sweden would be 3 to 15 times higher and that graph would look very different. Yet people continue to talk as if lockdowns were the only way to prevent that from happening. In fact, as we shall see, most scientific papers about the effect of non-pharmaceutical interventions implicitly rest on that assumption. It’s as if reality didn’t matter, but it does, or at least it should.
The average number of COVID-19 deaths per capita for the EU without Sweden hides a significant amount of heterogeneity: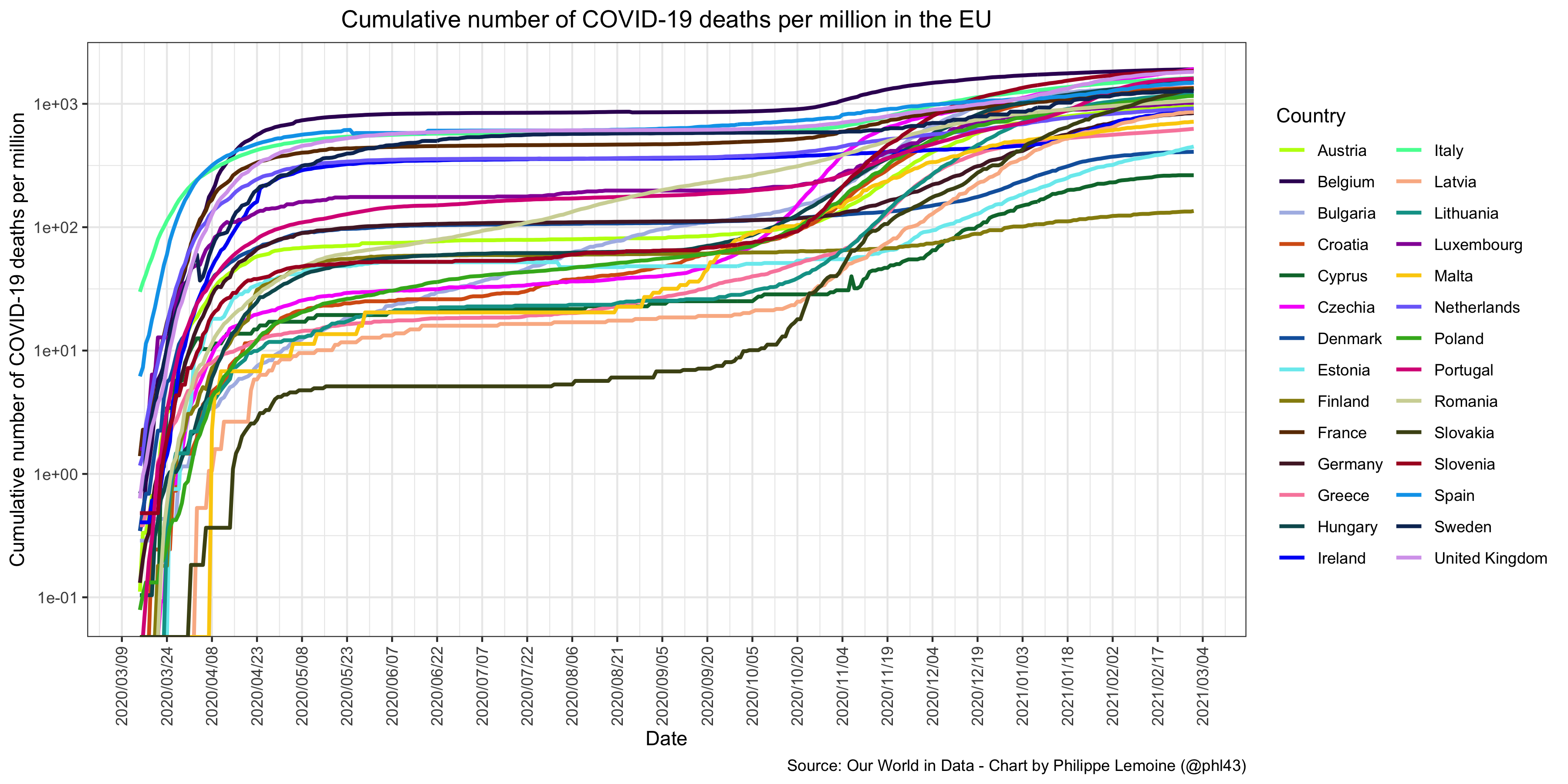 However, as you can see, the picture remains very similar even when you disaggregate and still shows a lot of convergence.
However, as you can see, the picture remains very similar even when you disaggregate and still shows a lot of convergence.
Moreover, although there remain significant disparities between EU countries, what is striking, if you have kept yourself informed about the various policies used to contain the epidemic in various EU countries, is the lack of any clear relationship between policy and outcomes: For instance, Finland is the country with the smallest number of COVID-19 deaths per capita, yet although it locked down last spring, restrictions in Finland have been even more relaxed than in the much-reviled Sweden for months. Of course, I’m not saying that you couldn’t find some kind of relationship if you looked close enough and used enough fancy statistics, but the point is precisely that you’d have to look very close.
For instance, Finland is the country with the smallest number of COVID-19 deaths per capita, yet although it locked down last spring, restrictions in Finland have been even more relaxed than in the much-reviled Sweden for months. Of course, I’m not saying that you couldn’t find some kind of relationship if you looked close enough and used enough fancy statistics, but the point is precisely that you’d have to look very close.
The situation is very similar in the US. You may recall that, back in April, The Atlantic published a piece called “Georgia’s Experiment in Human Sacrifice“ decrying the decision by the governor of that state to lift many restrictions. So let’s have a look at the result of this so-called experiment: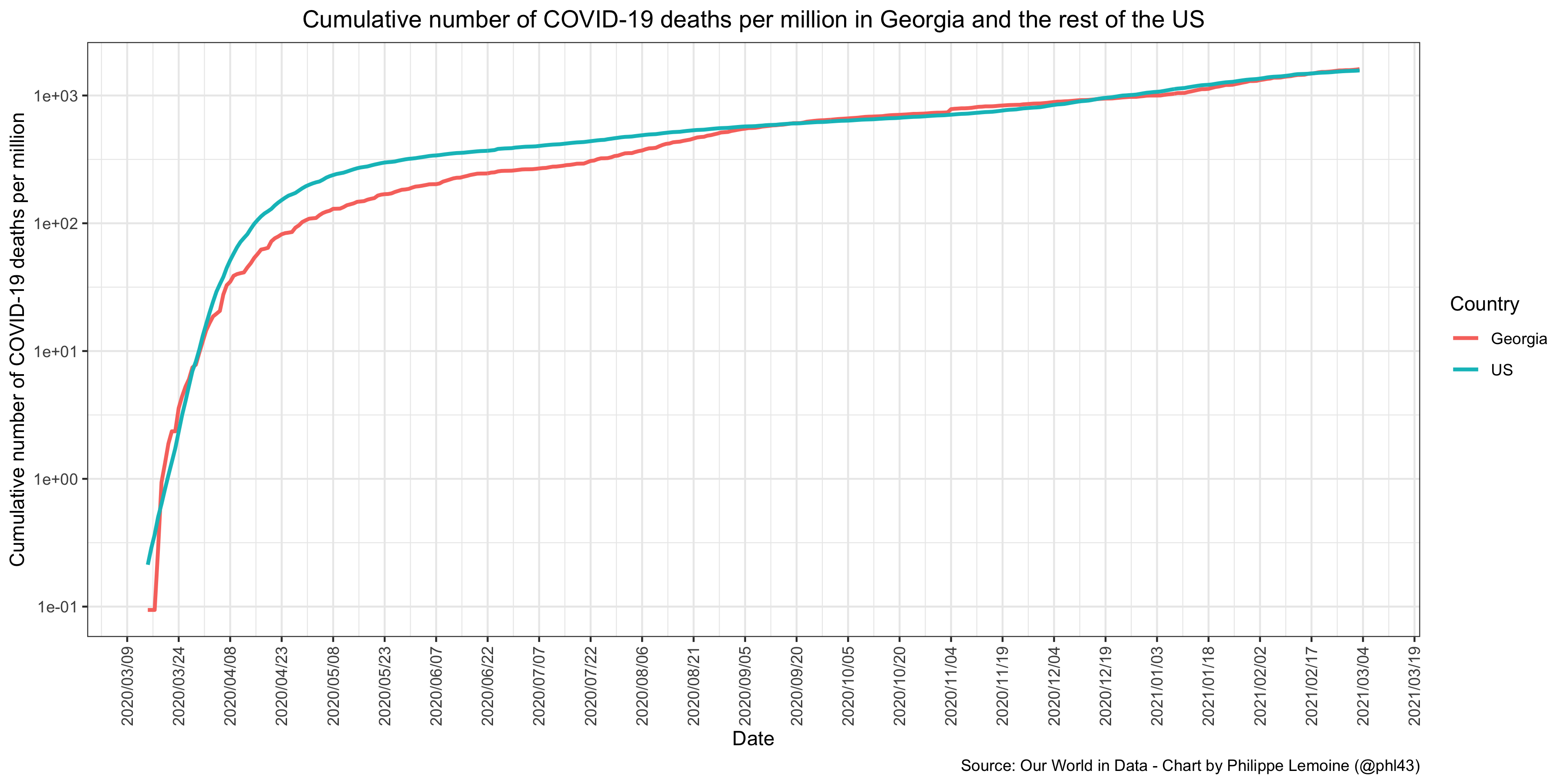 As you can see, the number of COVID-19 deaths per capita did increase and eventually caught up with the average of the US (although this graph doesn’t show any clear effect of Governor Kemp’s decision to lift many restrictions at the end of April), but the carnage predicted by opponents of that decision never happened and the number of COVID-19 deaths per capita in Georgia is actually slightly under the US average. Again, Georgia may have characteristics that protected it from a worse outcome and this graph obviously doesn’t show that the death toll would not have been lower with more stringent restrictions, but it still makes clear that policy isn’t as powerful a factor as Kemp’s critics assumed and as many people still assume.
As you can see, the number of COVID-19 deaths per capita did increase and eventually caught up with the average of the US (although this graph doesn’t show any clear effect of Governor Kemp’s decision to lift many restrictions at the end of April), but the carnage predicted by opponents of that decision never happened and the number of COVID-19 deaths per capita in Georgia is actually slightly under the US average. Again, Georgia may have characteristics that protected it from a worse outcome and this graph obviously doesn’t show that the death toll would not have been lower with more stringent restrictions, but it still makes clear that policy isn’t as powerful a factor as Kemp’s critics assumed and as many people still assume.
As in the case of the EU, if you disaggregate, the graph reveals a lot of heterogeneity between states, but the same pattern of convergence is also present: Some of the states that were relatively spared during the first wave remain less affected than average, but the difference has shrunk and, in many other cases, they have caught up with the US average and sometimes even exceed it.
Some of the states that were relatively spared during the first wave remain less affected than average, but the difference has shrunk and, in many other cases, they have caught up with the US average and sometimes even exceed it.
Again, although there remain significant disparities between states, the role of policy doesn’t jump out at you if you know what different states have done to deal with the pandemic: Again, I’m not saying that you couldn’t find a relationship with policy if you looked hard enough, but it would take some work and no amount of statistics should convince anyone who has seen those graphs that lockdowns and other stringent restrictions are the only way to prevent the virus from quickly sweeping through the population until saturation is reached.
Again, I’m not saying that you couldn’t find a relationship with policy if you looked hard enough, but it would take some work and no amount of statistics should convince anyone who has seen those graphs that lockdowns and other stringent restrictions are the only way to prevent the virus from quickly sweeping through the population until saturation is reached.
Even if someone has been able to find a large effect of non-pharmaceutical interventions on transmission with a more sophisticated statistical analysis, the fact it doesn’t jump at you when you look at this kind of simple graphs should make you skeptical of that finding and, the larger the effect, the more skeptical you should be, because if non-pharmaceutical interventions really had a very large effect it should be easy to see it without fancy statistics. I think that, in general, one should be very suspicious of any claim based on sophisticated statistical analysis that can’t already be made plausible just by visualizing the data in a straightforward way. (To be clear, this doesn’t mean that you should be very confident the effect is real if you can, which in many cases you shouldn’t.) That’s because sophisticated statistical techniques always rest on pretty strong assumptions that were not derived from the data and you should usually be more confident in what you can see in the data without any complicated statistical analysis than in the truth of those assumptions. So visualizing the data provides a good reality check against fancy statistical analysis. By following this principle, you will sometimes reject true results, but in my opinion you will far more often avoid accepting false ones. As we shall see later, not only is the literature on the effect of non-pharmaceutical interventions no exception, but it’s actually a great illustration of the wisdom of that principle.
Another way to convince yourself that, whatever the precise effect of lockdowns and other stringent restrictions, it’s almost certainly not huge is to compare the timing of non-pharmaceutical interventions with the evolution of the epidemic. Indeed, while you can find plenty of examples that are compatible with the pro-lockdown narrative, as long as you don’t cherry-pick the data, you can also find plenty of examples that are difficult to reconcile with that narrative. In particular, if you look at the data without preconceived notions instead of picking the examples that suit you and ignoring all the others, you will notice 3 things:
- In places that locked down, incidence often began to fall before the lockdown was in place or immediately after, which given the reporting delay and the incubation period means that the lockdown can’t be responsible for the fall of incidence or at least that incidence would have fallen even in the absence of a lockdown.
- Conversely, it’s often the case that it takes several days or even weeks after the start of a lockdown for incidence to start falling, which means that locking down was not sufficient to push
below 1 and that other factors had to do the job.
- Finally, there are plenty of places that did not lock down, but where the epidemic nevertheless receded long before the herd immunity threshold was reached even though incidence was increasing quasi-exponentially, meaning that even in the absence of a lockdown other factors can and often do cause incidence to fall long before saturation.
I’m just going to give a few examples for each category, but I could talk about many others in each case and, if you spend a bit of time looking at the data, you will have no problem finding more yourself.
A good example of a place where incidence started falling before the lockdown was in place is France during the second wave: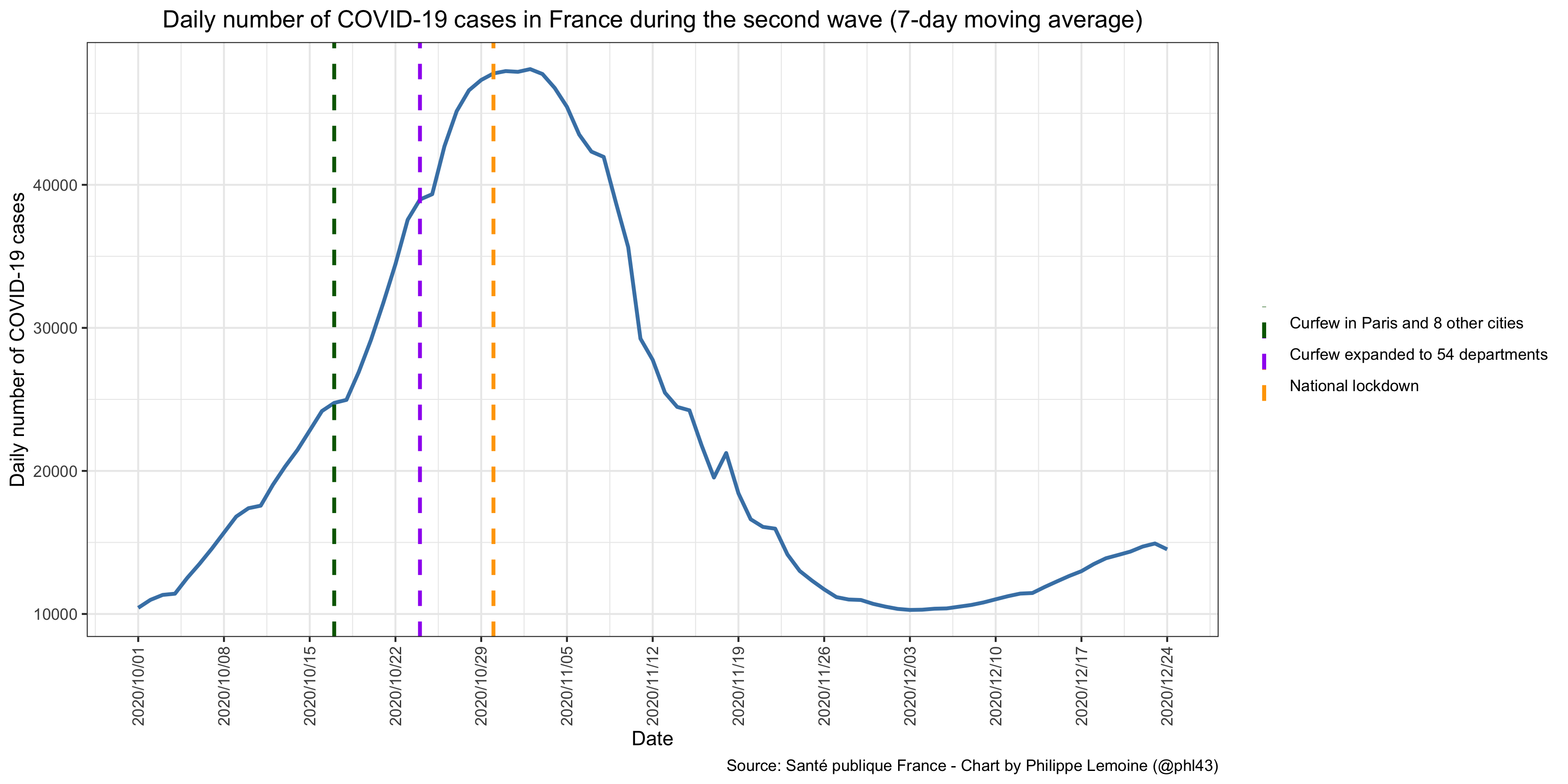 We can see clearly that had already stopped increasing by the time the lockdown came into effect.
We can see clearly that had already stopped increasing by the time the lockdown came into effect.
Since the incubation period lasts almost a week on average and people generally don’t get tested immediately after the onset of symptoms, there is absolutely no way the fall of incidence was due to the lockdown, although we can’t exclude that it accelerated the fall once it came into effect. Indeed, when you infer the number of infections from the data on death by using the infection-to-death distribution to reconstruct when people were infected based on when they died, you find that the peak was reached about a week before the lockdown started, even without taking into account the reporting delay in the data on deaths. This method is not very precise and the specific date of the peak shouldn’t be taken seriously, but it’s clear that incidence started falling before the lockdown. This is so obvious that it’s clear even in all-cause mortality data, which have the inconvenience of not including only deaths due to COVID-19, but the benefit of being higher-quality since deaths are recorded by date of death and not by date of report.
Yet another way to see that is to disaggregate the data geographically and look at different areas separately. For instance, if you look at the number of cases in Paris, you can clearly see that incidence started falling before the lockdown: As you can see, by the time the lockdown came into effect, incidence had already been falling for a few days. You could argue that it’s because of the curfew, though it’s unclear the timing is consistent with that hypothesis either and there are regions where incidence started falling before the lockdown despite the absence of curfew, but in any case it’s definitely not because of the lockdown.
As you can see, by the time the lockdown came into effect, incidence had already been falling for a few days. You could argue that it’s because of the curfew, though it’s unclear the timing is consistent with that hypothesis either and there are regions where incidence started falling before the lockdown despite the absence of curfew, but in any case it’s definitely not because of the lockdown.
Unfortunately, being as clueless as ever, the epidemiologists who advise the French government still don’t seem to have gotten the memo even 4 months later. Indeed, in a paper they recently published about machine learning models they created to predict the short-term evolution of the epidemic, they note that all of them “over-estimate the peak since the lockdown”, but claim it’s because the date of the lockdown “could not have been anticipated”, which is obviously not the explanation since again the peak of infections was reached before the lockdown. If you take another look at the graph for the country as a whole, it’s also interesting to note that incidence started to rise again about 2 weeks before the lockdown was lifted on December 15. You can say that it’s because people started to relax and this reduced compliance, but you don’t actually know that and, even if that were true, it’s the effectiveness of the actual lockdown that we’re interested in, not a theoretical lockdown where compliance remains the same throughout. Indeed, you can’t ignore the problem of non-compliance, which becomes even more important as time goes by and “lockdown fatigue” sets in.
The UK during the second wave also provides a very interesting example, even though it’s not clear that incidence started falling before the second national lockdown started on November 5. Indeed, the Office for National Statistics has been conducting the COVID-19 Infection Survey, a repeated cross-sectional survey of SARS-CoV-2 swab-positivity in random samples of the population since last May, so we have much better data to follow changes in incidence than in other countries, where we have to rely on data on non-random tests that are extremely noisy and subject to various biases. Here is a chart from the December 11, 2020 report, which shows the proportion of people in England that tested positive in that survey: If you look at the point estimates, the peak was reached during the week between November 8 and November 14, but the confidence intervals of the estimate overlap for any week between October 17 and November 21, so we can’t rule out the hypothesis that it was reached before the lockdown started. But regardless of when exactly the peak was reached, what is certain from this graph is that the growth rate of positivity started to collapse long before the lockdown started, so there is every reason to believe that incidence would have fallen even without a lockdown.
If you look at the point estimates, the peak was reached during the week between November 8 and November 14, but the confidence intervals of the estimate overlap for any week between October 17 and November 21, so we can’t rule out the hypothesis that it was reached before the lockdown started. But regardless of when exactly the peak was reached, what is certain from this graph is that the growth rate of positivity started to collapse long before the lockdown started, so there is every reason to believe that incidence would have fallen even without a lockdown.
If you look at the results disaggregated by region in the same report, it does look as though positivity started to fall before the lockdown in some regions: However, since a three-tiered framework of restrictions had been introduced in October, it could be argued that the decline in positivity was due to the restrictions that were implemented in those regions before the lockdown came into effect. (The same thing could be said about France during the second wave, where a curfew was put in place in some regions before a national lockdown was implemented.) What is more interesting is that, in several regions, the lockdown is not clearly associated with any change in positivity, which is hard to reconcile with the hypothesis that lockdowns and stringent restrictions have a very large effect. Although those results involve a lot of modeling and shouldn’t be taken at face value, this is another thing that we see again and again in the data of several countries when they are disaggregated by region, which has been largely ignored even though, or perhaps because, it’s at odds with the pro-lockdown narrative.
However, since a three-tiered framework of restrictions had been introduced in October, it could be argued that the decline in positivity was due to the restrictions that were implemented in those regions before the lockdown came into effect. (The same thing could be said about France during the second wave, where a curfew was put in place in some regions before a national lockdown was implemented.) What is more interesting is that, in several regions, the lockdown is not clearly associated with any change in positivity, which is hard to reconcile with the hypothesis that lockdowns and stringent restrictions have a very large effect. Although those results involve a lot of modeling and shouldn’t be taken at face value, this is another thing that we see again and again in the data of several countries when they are disaggregated by region, which has been largely ignored even though, or perhaps because, it’s at odds with the pro-lockdown narrative.
Next, let’s move to the second type of phenomenon I identified above, namely places where a lockdown was implemented but wasn’t associated with any fall of incidence. The most striking example of that phenomenon is arguably Peru, which had the worst epidemic in the world despite locking down very early: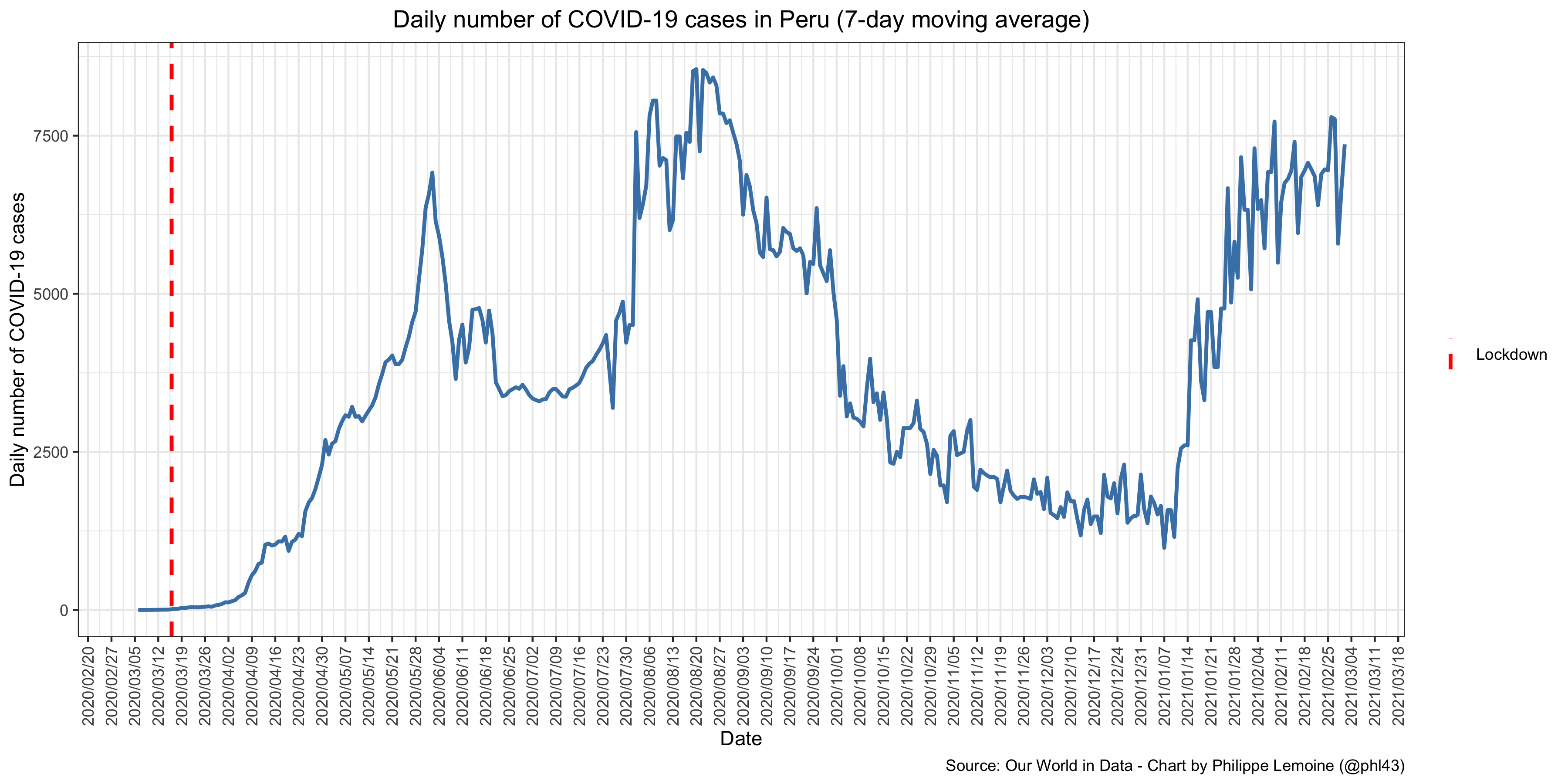 Pro-lockdown advocates like to insist that lockdowns are most effective when they are done early and the rules are stringent. Peru went on lockdown merely 9 days after the first case and before anyone had even died of COVID-19. Moreover, with the exception of China, the rules were stricter than anywhere else in the world and the government tightened them several times during the first 2 weeks of the lockdown. At one point, only men were allowed to leave their home on certain days and only women the rest of the week, while nobody was allowed to do so on Sunday. Grocery stores had to close at 3pm and the military was patrolling the streets to enforce the curfew. If there is one country where a lockdown should have prevented the epidemic from getting out of control, it was Peru, but it instead had the world’s highest known excess mortality rate in 2020.
Pro-lockdown advocates like to insist that lockdowns are most effective when they are done early and the rules are stringent. Peru went on lockdown merely 9 days after the first case and before anyone had even died of COVID-19. Moreover, with the exception of China, the rules were stricter than anywhere else in the world and the government tightened them several times during the first 2 weeks of the lockdown. At one point, only men were allowed to leave their home on certain days and only women the rest of the week, while nobody was allowed to do so on Sunday. Grocery stores had to close at 3pm and the military was patrolling the streets to enforce the curfew. If there is one country where a lockdown should have prevented the epidemic from getting out of control, it was Peru, but it instead had the world’s highest known excess mortality rate in 2020.
There are other examples of lockdowns that didn’t show any clear effect. Ironically, one of them is the lockdown in Melbourne that started in July and is often cited as an example by proponents of the so-called “zero covid” strategy, but I will discuss that later. Rather than look at clear-cut examples, I would like to discuss the third national lockdown in the UK, which is a very interesting case because, depending on what data you look at, you can argue that incidence started to fall immediately after it came into effect, that it started to fall before that or that it didn’t start to fall until much later. Thus, it illustrates the danger of inferring that a lockdown “worked” by visually inspecting a chart that shows the daily number of cases and noticing that it started falling shortly after the lockdown came into effect, as pro-lockdown advocates constantly do. Indeed, if you look at a graph showing the daily number of cases in England during the third wave, it certainly looks as though the lockdown worked exactly as expected: As you can see, the daily number of cases peaked a few days after the lockdown came into effect, which given the average incubation period seems roughly consistent with the hypothesis that transmission was suddenly cut by the lockdown.
As you can see, the daily number of cases peaked a few days after the lockdown came into effect, which given the average incubation period seems roughly consistent with the hypothesis that transmission was suddenly cut by the lockdown.
This is the graph most pro-lockdown advocates are looking at and the inference they make, but it doesn’t account for the reporting delay, which pushes back further the time when incidence started falling. Fortunately, the Office for National Statistics also publish data on the number of cases by date of specimen, so we can plot the daily number of cases without the reporting delay: As you can see, this tells a different story, since it shows that the number of cases actually started falling a few days before the lockdown came into effect. Since the incubation period lasts almost a week on average and people generally don’t get tested immediately after symptoms onset, this suggests that the number of infections started to fall at least a week before the lockdown came into effect, which would make England during the third wave another example of the first type of phenomenon I identified above.
As you can see, this tells a different story, since it shows that the number of cases actually started falling a few days before the lockdown came into effect. Since the incubation period lasts almost a week on average and people generally don’t get tested immediately after symptoms onset, this suggests that the number of infections started to fall at least a week before the lockdown came into effect, which would make England during the third wave another example of the first type of phenomenon I identified above.
Remarkably, when you disaggregate and look at the same data by region, every region exhibits a very similar pattern: This is remarkable because, on December 19, new restrictions were applied to London and parts of the East and South East that in some ways prefigured the lockdown, so if stringent restrictions had a large effect you would expect to see more pronounced differences between regions. It does look as though infections started to fall a little bit sooner and then fell a little bit faster in the regions where more stringent restrictions were in place, but the effect is hardly impressive and, as I will explain later, the results doesn’t mean that it was causal and there are good reasons to doubt that it was.
This is remarkable because, on December 19, new restrictions were applied to London and parts of the East and South East that in some ways prefigured the lockdown, so if stringent restrictions had a large effect you would expect to see more pronounced differences between regions. It does look as though infections started to fall a little bit sooner and then fell a little bit faster in the regions where more stringent restrictions were in place, but the effect is hardly impressive and, as I will explain later, the results doesn’t mean that it was causal and there are good reasons to doubt that it was.
But things are even more complicated with the third national lockdown in the UK. Indeed, while it looks as though incidence started to fall before the lockdown came into effect when you look at the data on cases, the REACT-1 study, another repeated cross-sectional survey of SARS-CoV-2 swab-positivity in random samples of the population of England whose 8th round was conducted in the 2 weeks following the beginning of the lockdown, didn’t find any fall in the positivity rate immediately after the lockdown started: As you can see, the positivity rate didn’t start falling until January 16, more than 10 days after the lockdown came into effect. Even taking into account the time it takes between the moment someone is infected and the moment the virus has replicated enough for a PCR test to come back positive, this seems too late for the lockdown to explain it. The authors of the report suggests that it may be due to a temporary increase in household transmission driven by the start of lockdown, as people started to spend more time with their family, but this is merely a conjecture and, as the report also notes, data on mobility don’t show any effect of the lockdown.
As you can see, the positivity rate didn’t start falling until January 16, more than 10 days after the lockdown came into effect. Even taking into account the time it takes between the moment someone is infected and the moment the virus has replicated enough for a PCR test to come back positive, this seems too late for the lockdown to explain it. The authors of the report suggests that it may be due to a temporary increase in household transmission driven by the start of lockdown, as people started to spend more time with their family, but this is merely a conjecture and, as the report also notes, data on mobility don’t show any effect of the lockdown.
The results disaggregated by region are once again show a diversity of patterns that is hard to reconcile with the hypothesis that restrictions have a huge effect on transmission: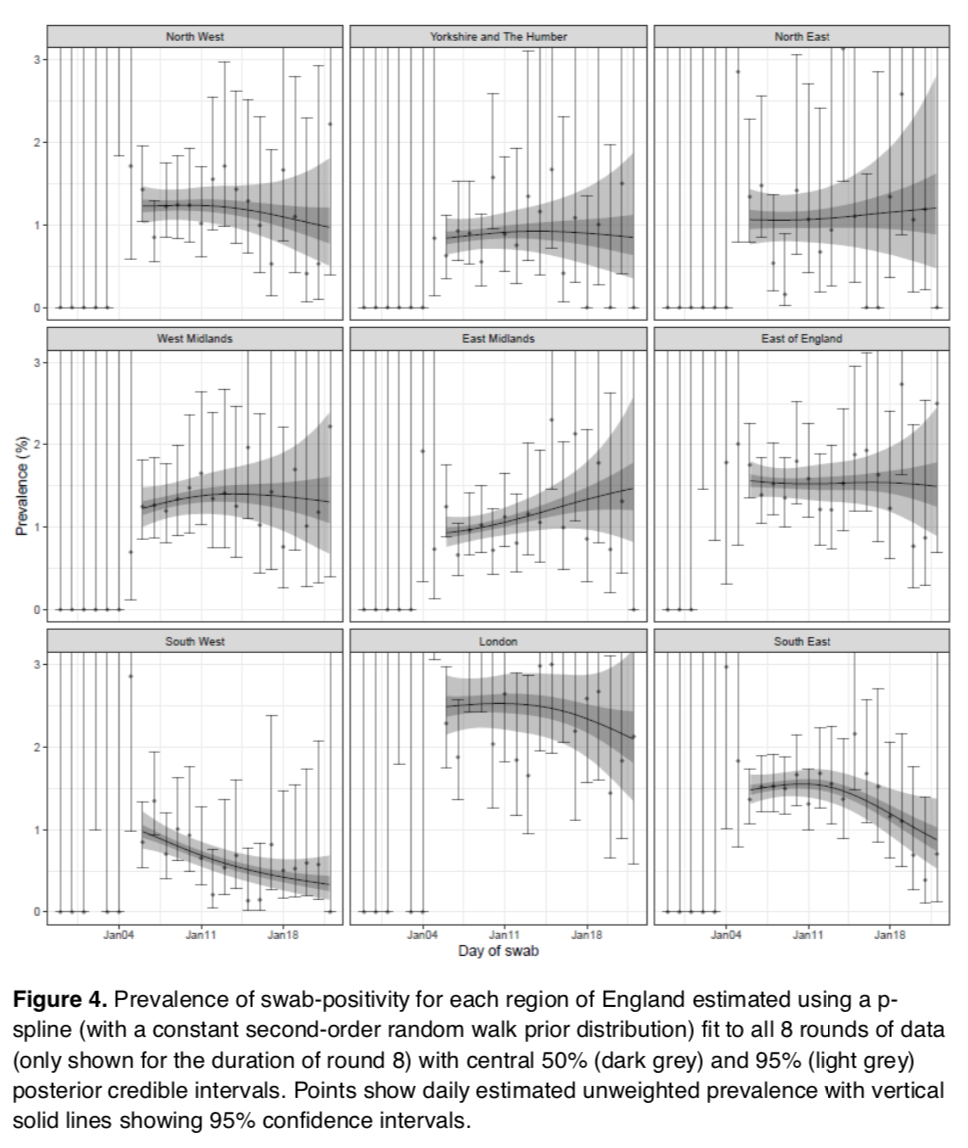 As you can see, in most regions the positivity rate doesn’t seem to have decreased much or at all even 2 weeks after the beginning of the lockdown, except in South West where robustly decreasing prevalence can be observed and East Midlands where prevalence actually seems to have increased during that period. I don’t see how anyone can look at those data and conclude that the lockdown was the main factor driving the epidemic in England during that period, which is probably why pro-lockdown advocates generally ignore them.
As you can see, in most regions the positivity rate doesn’t seem to have decreased much or at all even 2 weeks after the beginning of the lockdown, except in South West where robustly decreasing prevalence can be observed and East Midlands where prevalence actually seems to have increased during that period. I don’t see how anyone can look at those data and conclude that the lockdown was the main factor driving the epidemic in England during that period, which is probably why pro-lockdown advocates generally ignore them.
The COVID-19 Infection Survey also found a great deal of heterogeneity in the trajectory of the positivity rate in different regions, which is not what you’d expect if the lockdown had a massive effect on transmission: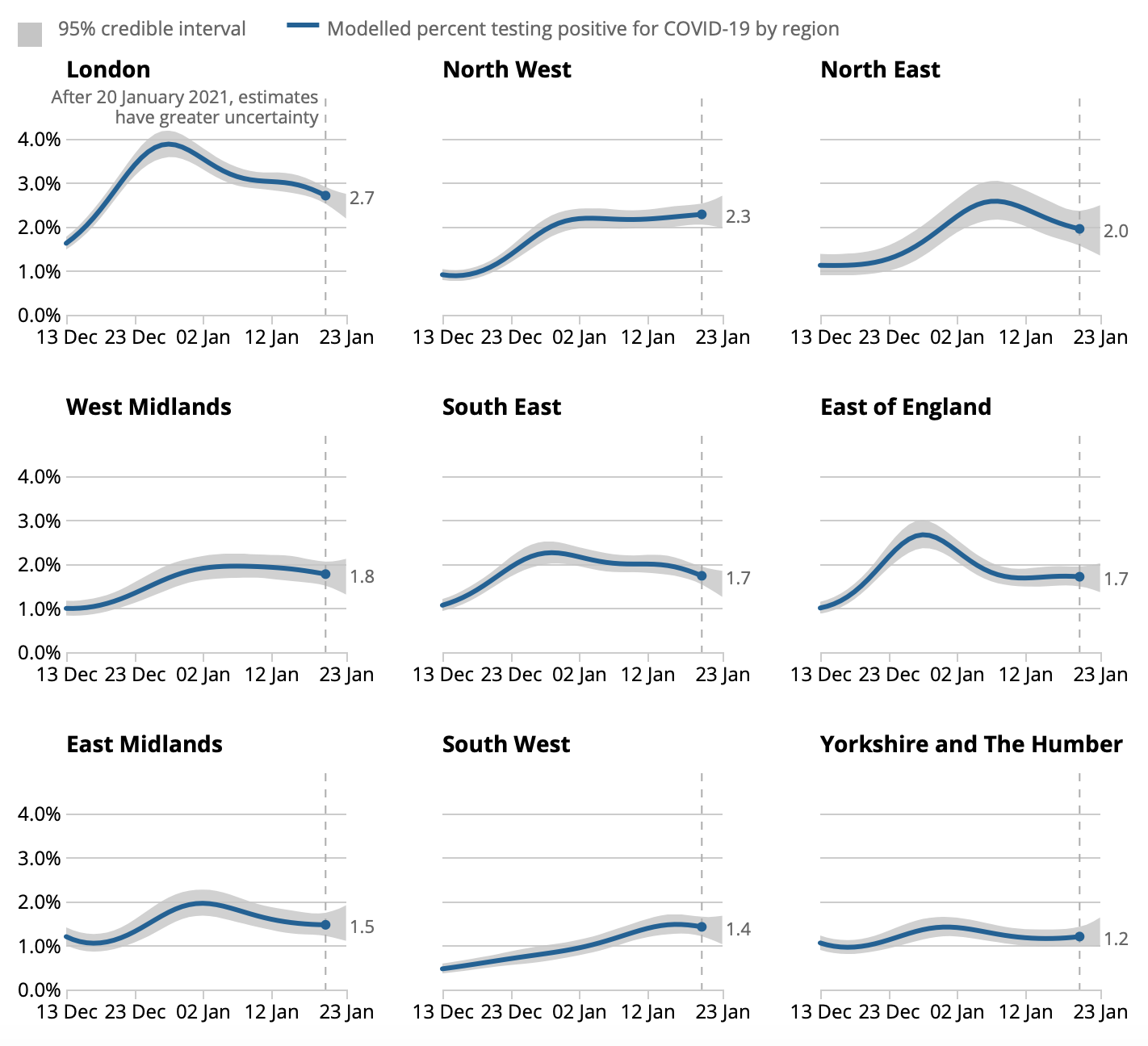 It’s also remarkable that, in several regions, the results are strikingly different from what the REACT-1 study shows. Of course, the results are not straightforwardly comparable, if only because the COVID-19 Infection Survey uses a different modeling approach. But the fact that you can get such different results is still pretty telling, because if the lockdown really had the kind of massive effect that pro-lockdown advocates claim, not only would you see a more homogenous response across regions, but differences in modeling choices presumably wouldn’t result in such inconsistent results.
It’s also remarkable that, in several regions, the results are strikingly different from what the REACT-1 study shows. Of course, the results are not straightforwardly comparable, if only because the COVID-19 Infection Survey uses a different modeling approach. But the fact that you can get such different results is still pretty telling, because if the lockdown really had the kind of massive effect that pro-lockdown advocates claim, not only would you see a more homogenous response across regions, but differences in modeling choices presumably wouldn’t result in such inconsistent results.
But what’s even more striking is that data from repeated cross-sectional surveys of SARS-CoV-2 swab-positivity in random samples of the population tell a completely different story from data on cases, which as we have seen suggest that incidence started falling everywhere about a week before the lockdown started. There are many possible explanations for this apparent inconsistency. For instance, it could be that infections started to fall earlier among older people, who are more likely to be symptomatic and get tested, but continued to increase among younger people for some time. However, this is not what the data from the COVID-19 Infection Survey show, so it probably isn’t the explanation. Another possible explanation is that data from the REACT-1 study and the COVID-19 Infection Survey, even though they rely on random samples of the population, are not very good. Indeed, the response rate seems pretty low in both cases, so inferring the prevalence of infection in the population from the sample may be misleading. Moreover, testing by PCR can detect viral RNA in swabs for a while after the infection was successfully fought off by the immune system, which probably makes it difficult to pick up small, gradual changes in prevalence even in a large sample. Of course, the problem could still come from the data on cases, it’s possible that something other than age changed among the people who were infected that resulted in a fall of the number of cases even though the number of infections was still increasing or staying roughly constant.
I spent some time on the case of the third national lockdown in England because it illustrates that, even when it looks as though a lockdown is clearly working, things get a lot muddier when you take a closer look at the data. The case of England is particularly interesting because, unlike in many places where only the data on the number of cases by date of report are available, we have lot of different sources of data on the epidemic in England, but I’m sure we’d reach a similar conclusion elsewhere if we had more data. The truth is that, based on the data we have, it’s impossible to tell whether the number of infections started to fall before, shortly after or as late as 10 days after the lockdown came into effect. Note that I’m just talking about what we can tell about the timing of the epidemic relative to that of the lockdown here, but as I will explain later, we couldn’t infer that the lockdown was responsible even if we knew for sure that incidence started to fall shortly after it came into effect, so the pro-lockdown case is even weaker than it looks. In general, I hope this discussion has illustrated how incredibly noisy the data about the pandemic are, even in the UK which has much better data than virtually any other country. This is important because all the studies that people tout as proof that lockdowns and other stringent restrictions have a huge effect on transmission are based on such very low-quality data, but I will go back to the scientific literature on the effect of non-pharmaceutical interventions later.
For the moment, I would like to turn to the third type of phenomenon I identified above, namely places that didn’t lock down but where incidence nevertheless started falling after a period of quasi-exponential growth. Examples of this type are for me the most important because they show that, even without a lockdown and with far less stringent restrictions than those currently in place in France and many other countries, a phase of quasi-exponential growth of incidence never lasts very long and the epidemic always ends up receding long before the herd immunity threshold is reached. The best known example is of course Sweden, which has never locked down and where restrictions are much less stringent than almost anywhere else in Europe, but where incidence didn’t continue to increase exponentially until the herd immunity threshold was reached but actually started to fall way before that, be it during the first wave last spring or during the second wave this winter: The data on cases are misleading for the first wave, because Sweden was testing very little at the time, so it looks as though incidence remained low, but the data on ICU admissions show very clearly that’s not what happened. What is also clear is that, despite the lack of lockdown or very stringent restrictions, the epidemic quickly reached its peak and began to decline by the beginning of April. For the second wave, Christmas and New Year’s Day clearly affected the data on cases, but we can still see that incidence declined for several weeks starting from the end of 2020 (even though it recently started to increase again), a conclusion that is further strengthened by the data on ICU admissions. As during the first wave, the epidemic eventually receded without a lockdown or a curfew and while small businesses, bars and restaurants remained open, even though the sale of alcohol is prohibited from 8pm onwards and a number of restrictions are still in place.
The data on cases are misleading for the first wave, because Sweden was testing very little at the time, so it looks as though incidence remained low, but the data on ICU admissions show very clearly that’s not what happened. What is also clear is that, despite the lack of lockdown or very stringent restrictions, the epidemic quickly reached its peak and began to decline by the beginning of April. For the second wave, Christmas and New Year’s Day clearly affected the data on cases, but we can still see that incidence declined for several weeks starting from the end of 2020 (even though it recently started to increase again), a conclusion that is further strengthened by the data on ICU admissions. As during the first wave, the epidemic eventually receded without a lockdown or a curfew and while small businesses, bars and restaurants remained open, even though the sale of alcohol is prohibited from 8pm onwards and a number of restrictions are still in place.
Many people think that Sweden is unique, but that’s not the case at all, there are many other places beside Sweden that have not locked down and where the epidemic still ended up receding long before saturation. For example, it’s what happened in Serbia this fall, where there was no curfew and bars and restaurants remained open during the week even at the height of the second wave, even though they had to close earlier than usual on weekdays and completely on weekends: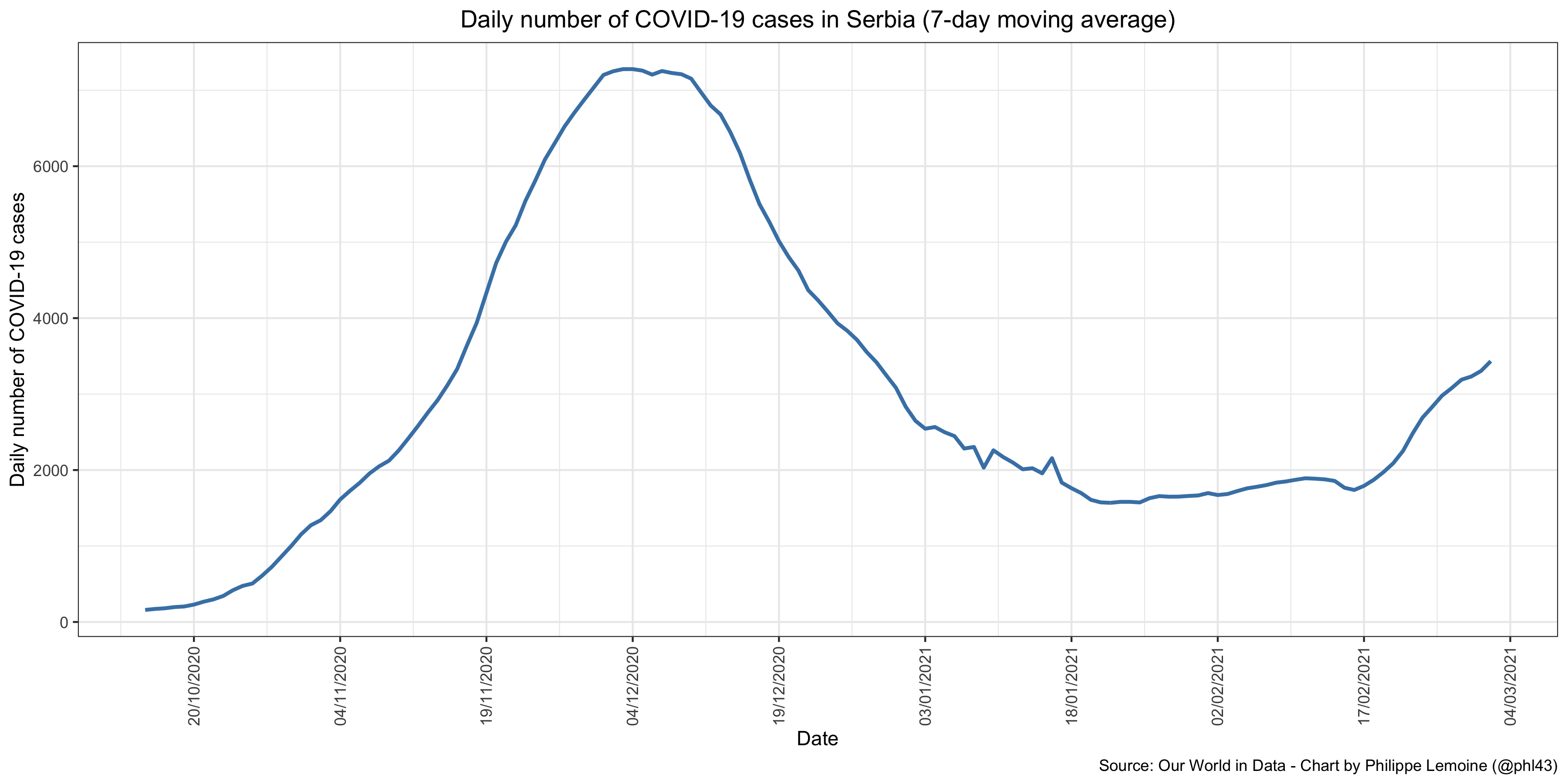 Again, it’s not as if there were no restrictions in Serbia, but they are much less stringent than in France and most other European countries. However, this didn’t prevent the epidemic from receding, even though it is clear that the country is very far from having reached the herd immunity threshold. Recently, incidence started increasing again, but it does not change what happened before and this is perfectly consistent with the explanation I will propose in the next section.
Again, it’s not as if there were no restrictions in Serbia, but they are much less stringent than in France and most other European countries. However, this didn’t prevent the epidemic from receding, even though it is clear that the country is very far from having reached the herd immunity threshold. Recently, incidence started increasing again, but it does not change what happened before and this is perfectly consistent with the explanation I will propose in the next section.
In the US, many states also refused to lock down after the first wave, but that didn’t stop the epidemic from eventually receding everywhere. For instance, this is what happened in Florida, one of the most populous states in the US, both last summer and this winter: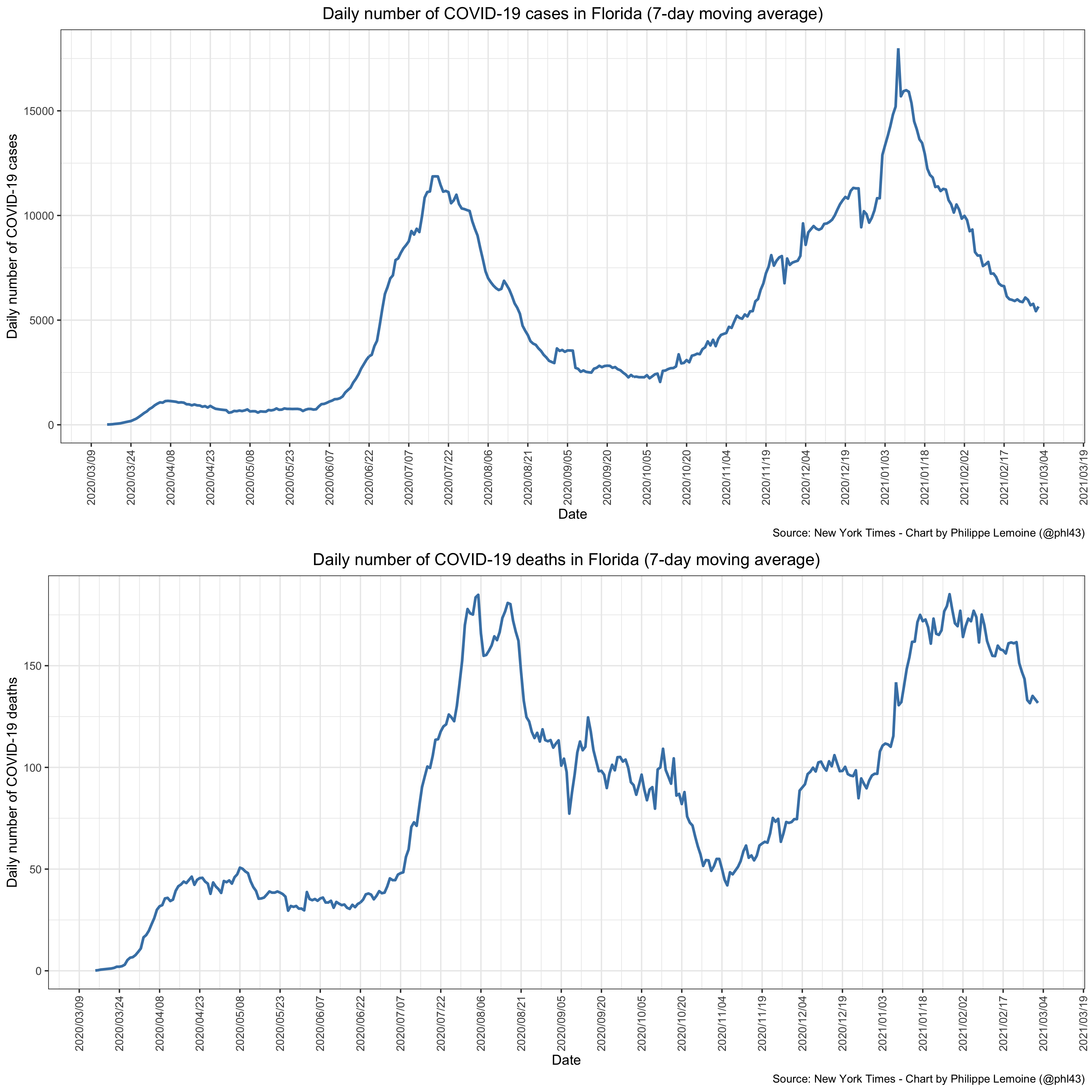 I also show the daily number of deaths because, like everywhere else, Florida tested very little during the first wave and the data on cases are therefore misleading.
I also show the daily number of deaths because, like everywhere else, Florida tested very little during the first wave and the data on cases are therefore misleading.
Florida did lock down in April, but since then Ron DeSantis, the state’s governor, has refused to do it again. Even at the height of the second wave, bars and restaurants remained open and there was no curfew except in Miami-Dade County, although the sale of alcohol was banned in bars at the end of June. In September, the governor ordered that all health restrictions be lifted in bars and restaurants, prohibiting even counties and cities from imposing such restrictions locally, which did not result in a resurgence of cases. When incidence began to rise again in November, despite the fact that experts and the media demanded that he impose stringent restrictions again, he refused to give in and the state remained completely open. Nevertheless, as you can see on the graph, the third wave also started to recede at the beginning of the year and incidence in Florida has been steadily falling since then. While there have been almost no restrictions since September, which actually makes Florida a far more extreme counter-example to the pro-lockdown narrative than Sweden, the cumulative number of deaths per capita in that state is barely higher than in France, where there is a curfew of 6pm, bars and restaurants have been closed everywhere since the end of October, etc. One could make a similar comparison with other European countries where restrictions have been very stringent or, as we shall see, with California, where restrictions are also far more stringent and where there even was a lockdown.
I could go on like that for hours, because there are plenty of examples that contradict the claim that, without a lockdown, incidence continues to rise quasi-exponentially until the herd immunity threshold is reached. Not only is this patently false, but in developed countries at least (I will go back to this point below), the epidemic ended up receding long before that point in every place that did not lock down, without a single exception. Unfortunately, most people don’t know that, because there is a huge bias in the way the media and people on social networks talk about the pandemic. For example, as long as the incidence was rising very rapidly in Sweden, I would see graphs every day showing the explosion of cases accompanied by alarmist and/or sarcastic commentary about the Swedish strategy, but curiously since incidence started falling I don’t hear about Sweden anymore. It’s the same thing with Florida, North Dakota, South Dakota, Georgia and every other place that did not lock down and where almost everything remained open even at the height of the second and/or third waves. Similarly, almost nobody has ever heard about what happened in Serbia, which adopted a strategy very similar to that of Sweden during the second wave.
Conversely, when a lockdown or stringent restrictions fail to quickly produce visible results, as in California last December, you don’t hear from that place again until incidence finally starts falling, which again it always does eventually with or without a lockdown or stringent restrictions. At which point, you start hearing about that place again, which becomes the latest proof that lockdowns are effective even though it’s hardly obvious upon taking a close look at the data, as we have seen in the case of the third national lockdown in England. When a lockdown has failed to produce any visible results even after 2 weeks, but the media can’t ignore it for one reason or another, we are assured that it’s because it wasn’t strict enough. Of course, pro-lockdown advocates never say in advance what restrictions will be stringent enough, nor after how long we may conclude that they didn’t work, so they can never lose.
When incidence starts rising again in places that have not locked down, which will probably happen in at least some of them, the same people who had forgotten their existence will start talking about the “Swedish disaster“ or the “Georgia’s experiment in human sacrifice“ again. Cases that support the view that only very stringent restrictions can prevent a disaster are talked about constantly, while any counter-example to that view is systematically ignored. For the most part, people are not even being intellectually dishonest, it’s just confirmation bias on steroids. This is made worse by the fact that the issue has been politicized, though not always along traditional political divides, so people have to toe the party line. I know many people who understand what I’m saying perfectly well, but they will never say it publicly or say it in a much watered down form, because they’re afraid of what people on their team would think. The issue of lockdowns has practically become a religion for some people and they do not easily forgive slights to their god.
When you point out counter-examples to their view, pro-lockdown individuals always have a way to explain them away. They are always ready to bring up a difference, real or imagined, between places that have not locked down and others that did not which they believe explains why the epidemic wasn’t significantly worse in the former than in the latter. In the case of Sweden, what always comes up is population density. If Sweden did not have more COVID-19 deaths than many countries that have put in place far more stringent restrictions, so the argument goes, it’s because it has a very low population density. The problem is that, when you look at the data, there is no clear relationship between population density and the number of COVID-19 deaths per capita: I have restricted myself to Europe, which is relatively homogeneous in demographic and economic terms, to reduce the risk that even a strong association between population density and the number of COVID-19 deaths per capita be hidden by other, even more important factors, such as the proportion of the population over 60. (I would like to thank Antoine Lévy for providing me with this dataset, which he constructed for the purposes of his analysis in a recent paper, but it goes without saying that none of the opinions I express in this post should be attributed to him.) I also used population-weighted population density rather than population density, because population density is often extremely misleading because even in a very large country, people are usually concentrated in a tiny part of the territory.
I have restricted myself to Europe, which is relatively homogeneous in demographic and economic terms, to reduce the risk that even a strong association between population density and the number of COVID-19 deaths per capita be hidden by other, even more important factors, such as the proportion of the population over 60. (I would like to thank Antoine Lévy for providing me with this dataset, which he constructed for the purposes of his analysis in a recent paper, but it goes without saying that none of the opinions I express in this post should be attributed to him.) I also used population-weighted population density rather than population density, because population density is often extremely misleading because even in a very large country, people are usually concentrated in a tiny part of the territory.
As you can see on this graph, even when you restrict yourself to a group of countries that are relatively homogenous in economic, cultural and demographic terms, there is no clear relationship between population density and the number of COVID-19 deaths per capita. You can also see that Serbia, where as I have already noted the second wave has receded without a lockdown, has a population-weighted population density roughly equal to that of France and other countries where pro-lockdown advocates assure us Sweden’s strategy could never work because population density is higher. The same thing could be said about many other places, such as Florida, where the same thing happened. Of course, it doesn’t mean that, other things being equal, population density doesn’t result in higher transmission and in fact I have no doubt that it does, but clearly the effect is not as large as one might have thought, otherwise it would be easier to detect. This example illustrates a recurring phenomenon in debates about the pandemic. People make wild conjectures that often aren’t even supported by the data we have, but assert them as if they were established fact. We’ll see another example of this phenomenon when I briefly discuss what happened in Asian countries that managed to keep the epidemic under control without lockdowns.
Another argument that is often made is that you shouldn’t compare Sweden to countries like France, the UK or Belgium but only to its neighbors, because due to cultural proximity or whatever they provide a better counterfactual of what would have happened in Sweden if the government had decided to lock down. However, as I explained elsewhere, not only is this claim largely gratuitous, but it’s demonstrably false. Indeed, when you infer the number of infections during the first wave from the number of deaths, you find that, by the time its neighbors decided to lock down, the epidemic was already far more advanced in Sweden. Thus, even if Sweden had locked down around the same time as its neighbors and we assume that it would have suddenly cut transmission by a very large factor, which as we have seen is almost certainly false, there would still have been far more COVID-19 deaths in Sweden because a lot more people had already been infected and it would have taken longer for incidence to go down since it was starting from a much higher level. Frankly, it’s incredible that so many people still believe that policy explains most of the difference in outcomes between Sweden and its neighbors. Even if I were wrong about what happened during the first wave, as I already noted, Finland remains almost entirely spared by the pandemic even though restrictions have been even less stringent than in Sweden for months. The same thing could be said about most of Norway. Although nobody knows what they are, there are clearly factors beyond policy that play a major role and explain why Sweden’s neighbors have largely been spared by the pandemic, but people continue to make this comparison as if it proved that Sweden’s failure to lock down explains most of the difference.
Pro-lockdown advocates like to bring up culture to explain away inconvenient facts, but while I have no doubt that culture affects the course of the epidemic, cultural explanations have repeatedly proved wrong since the beginning of the pandemic, without reducing people’s appetite for them. For instance, when it became clear that the holocaust that pro-lockdown advocates predicted in Sweden had failed to materialize and that COVID-19 mortality was not particularly high over there, many of them started to say that Sweden’s strategy could not be replicated in other countries not just because of population density but also because they lacked the Swedish culture of compliance with government rules. Thus, when incidence started to explode in Spain a few weeks ago and the government refused to lock down (it even prevented local governments from locking down when they tried), they naturally denounced that decision as irresponsible, since what Sweden did could never be replicated in a Latin country such as Spain. Instead, I predicted that incidence would soon begin to fall, which is exactly what happened: In fact, although I couldn’t have known it when I made that prediction, the number of cases had already started to fall. That’s because data on cases by date of symptoms onset take a while to be compiled, so we only had data on cases by date of report and there is a significant reporting delay.
In fact, although I couldn’t have known it when I made that prediction, the number of cases had already started to fall. That’s because data on cases by date of symptoms onset take a while to be compiled, so we only had data on cases by date of report and there is a significant reporting delay.
Now that incidence has collapsed, some of the people who predicted the apocalypse have done a U-turn and now claim there was a de facto lockdown in Spain, on the ground that many regions had put in place stringent restrictions even though they were prevented by the national government from implementing a complete lockdown. But it’s still the case that almost everywhere in Spain restrictions were less stringent than in the UK or even France, which is not even locked down but where there is a curfew at 6pm and bars and restaurant are closed except for take-out. Moreover, in some regions (such as Madrid), restrictions remained very limited. Bars and restaurants were allowed to remain open at all time until January 18, 2021 when they were forced to close at 10pm, while a curfew starting at 11pm came into effect. On January 25, the closing time for bars and restaurants was changed to 9pm, while the curfew was advanced to 10pm. In other regions, restrictions were more stringent, sometimes a lot more, but again they remained less stringent than in France or the UK almost everywhere. Thus, I don’t see how anyone can seriously claim that Spain was de facto on lockdown when incidence started to fall, if by that we mean something like what the country did last Spring or what the UK or even France are currently doing. If pro-lockdown advocates in France or the UK really think that, then they should ask that bars and restaurants be reopened over there, but somehow I don’t think that’s going to happen.
Despite the fact that restrictions in Spain ranged from very limited as in Madrid to very stringent as in Murcia, incidence started to fall everywhere around the same time in January: You may be able to argue that it started to fall a bit earlier and that it has been falling a bit faster in regions with the most stringent restrictions in place, which doesn’t mean that it was because of that, but it still fell everywhere including in regions where restrictions were very limited. In fact, if you look at the timing of the fall and compare it to that of the restrictions in each region, you will generally find that incidence started to fall before the most stringent restrictions came into effect, especially when you take into account the period of incubation. So the prediction that Sweden’s strategy wouldn’t work in Spain because it doesn’t have the right culture proved spectacularly wrong.
You may be able to argue that it started to fall a bit earlier and that it has been falling a bit faster in regions with the most stringent restrictions in place, which doesn’t mean that it was because of that, but it still fell everywhere including in regions where restrictions were very limited. In fact, if you look at the timing of the fall and compare it to that of the restrictions in each region, you will generally find that incidence started to fall before the most stringent restrictions came into effect, especially when you take into account the period of incubation. So the prediction that Sweden’s strategy wouldn’t work in Spain because it doesn’t have the right culture proved spectacularly wrong.
I’m sure there are plenty of differences between the places that have locked down and those that have not, and even that some of them affect the epidemic, although the truth is that nobody knows what they are or how exactly they do so. But places that have not locked down or put in place very stringent restrictions are so diverse economically, culturally, demographically, etc. that if incidence nevertheless started to fall long before the herd immunity threshold was reached in all of them, it’s extremely unlikely that it’s because they all happen to have characteristics that make not locking down a viable option, whereas everywhere else this policy would lead to the disaster predicted by pro-lockdown advocates as incidence would continue to increase quasi-exponentially until the herd immunity threshold is reached. At this point we have so many examples, and no counter-examples, that such a claim is akin to magical thinking. It’s far more likely that, whenever and wherever incidence starts increasing quasi-exponentially somewhere, the same mechanisms push below 1 long before the herd immunity threshold is reached even when there is no lockdown or stringent restrictions. In the next section, I propose a theory of what this mechanism could be, which also explains why it often looks as though lockdowns and other stringent restrictions are very effective and why many governments have used them despite their cost and limited effectiveness.
A theory of why lockdowns and other stringent restrictions don’t make a huge difference
Many people assume that, without a lockdown, when incidence starts increasing quasi-exponentially, it will continue to rise in that way until the herd immunity threshold is reached. But as we have seen, this is not what happens and therefore it doesn’t make sense to extrapolate from current growth by assuming it will continue until something like 66% of the population has been infected. It’s true that, in a standard compartmental model, incidence rises quasi-exponentially until the attack rate approaches the herd immunity threshold, but that’s only the case when, among other things, the contact rate is assumed to be constant. However, with or without lockdown, the contact rate never remains constant because people respond to epidemic conditions by changing their behavior, which affects the contact rate and therefore also . (I will pass over the fact that, beyond the assumption that both the contact rate and the generation interval remain constant, which can easily be relaxed, the model from which the formula that everyone is using to compute the herd immunity threshold is totally unrealistic, in particular because it assumes a perfectly homogenous population, so that we don’t actually know what the herd immunity threshold really is.) Beside, even if this were not the case, given that
has been hovering between 1 and 1.5 for months almost everywhere, we’d still expect the epidemic to start receding long before 66% of the population has been reached anyway.
To the extent that restrictions have any effect on transmission, they presumably have both direct and indirect effects. Direct effects consist in physically preventing certain events that contribute to the spread of the virus. For example, if the government bans large gatherings and the ban is respected, it becomes physically impossible for a single person to infect hundreds of people at the same time. But presumably restrictions also have indirect effects because they send a signal to the population, which can translate into behavioral changes that in turn can affect the contact rate and/or the generation interval. (The contact rate is a quantity used to model how often people meet each other in a way that results in someone getting infected, while the generation interval is the time between the moment someone is infected and the moment they infect someone else.) My theory about the epidemic is that, once you have some basic restrictions in place, such as a ban on large gatherings, then unless perhaps you go very far as the Chinese authorities did in Wuhan (which I think is neither possible nor desirable in a democracy), more stringent restrictions have a rapidly decreasing marginal return because they are a very blunt instrument that has a hard time targeting the behaviors that contribute the most to transmission and people reduce those behaviors on their own in response to changes in epidemic conditions such as rising hospitalizations and deaths. However, as I explain below, it doesn’t mean that their marginal cost also decreases rapidly. For instance, a 6pm curfew as in France probably doesn’t have much impact if any on transmission, but it arguably has a large effect on people’s well-being.
In simple terms, what this means is that, once the authorities have put in place relatively limited restrictions, everything they do after that has an increasingly small effect on transmission and consequently the most stringent restrictions only have a relatively negligible impact on the dynamics of the epidemic. (Again, it’s plausible that it ceases to be true if you go very far as the Chinese authorities did in Wuhan, but even in China we don’t really know for sure that lockdowns were essential to the country’s ability to suppress the virus. Indeed, neighboring countries were able to do the same thing without lockdowns, so I don’t see why people are so confident that lockdowns are what did the work in China as opposed to whatever did the work in other East Asian countries.) If this were not the case, given how much variation in policy there is between regions, the graphs of the cumulative number of COVID-19 deaths in US states or European countries I have shown above would almost certainly look very different. On the other hand, there is very little variation in more limited non-pharmaceutical interventions such as bans on large gatherings, which are in place almost everywhere, so this doesn’t tell us they only have a small effect and I think we have good reasons to think they have a significant one even though ultimately even that is not clear. Again, I’m not claiming that lockdowns and other stringent restrictions have no effect on transmission, I’m just saying that when you look at the data it’s hard to convince yourself they have more than a relatively small effect and it’s impossible to maintain that it’s as large as pro-lockdown advocates claim.
Moreover, when I say that people’s voluntary behavior changes in response to changes in epidemic conditions, I’m not saying that the mechanism is necessarily just the aggregate reduction in social activity. For instance, since presumably not everybody respond in the same way to changes in epidemic conditions, it’s possible that a rise in incidence, which eventually results in a rise of hospitalizations and deaths that scare people into modifying their behavior, temporarily creates more heterogeneity in the population because some people will react more strongly to this change in epidemic conditions than others, which in turn lowers the herd immunity threshold until incidence goes down and eventually people go back to their previous behavior. One could also imagine that behavior changes increase the generation interval, which even keeping constant would lower the growth rate of the epidemic. Moreover, it’s likely that the type of social activity people engage in and not just how much of it they engage in matters a lot. If people disproportionately reduce the types of social activity that contribute the most to transmission, a relatively small reduction in aggregate social activity could result in a significant reduction in transmission.
In short, I make no hypothesis on the specific mechanisms underlying the feedback mechanism my theory posits at the micro-level, because I don’t think we really understand what’s going on at that level. I just claim that people’s behavior changes in response to changes in epidemic conditions and that whatever the specific mechanisms at the micro-level those behavior changes eventually make the epidemic recede even when a relatively small share of the population has been infected. Of course, I’m not claiming that the feedback mechanism posited by my theory is the only factor driving the dynamics of the epidemics, but I think it’s probably the main factor explaining why over and over again dropped below 1 in places where the prevalence of immunity just wasn’t high enough to explain that, as shown by the fact that eventually the epidemic blew up again. (There are other possible explanations and most of them aren’t even mutually exclusive with my theory, but for various reasons I won’t get into, I don’t think they can really explain the data.) However, at this point, I think the prevalence of immunity is high enough in many places that it can plausibly explain why incidence is falling even in the absence of any behavior changes. But I doubt that incidence wouldn’t start rising again if everyone returned to their pre-pandemic behavior.
My theory predicts that, in places where the IFR and the hospitalization rate are lower because the population is younger, the virus will be able to spread faster and the attack rate (i. e. the proportion of people who have been infected) will be higher. Indeed, if the feedback mechanism I postulate operates through exposure to information about the number of deaths and hospitalizations, people won’t start changing their behavior enough to push below 1 until the daily numbers of deaths and hospitalizations scare them. In a place where people are very young, incidence will have to rise much higher than in developed countries, where a large share of the population is over 60, before this happens. For example, pro-lockdown advocates often cite the case of Manaus, a Brazilian city where a study concluded that about 75% of the population had already been infected by October, which didn’t prevent another wave at the beginning of the year. First, I think it’s extremely implausible that 75% of the population had really been infected at the time, since the study is based on a non-random sample and that estimate was obtained after significant corrections to account for antibody waning, while seropositivity never exceeded 44% in any sample. (I also think it’s a bad idea to generalize from what seems like a clear outlier, but let’s put that aside.) In any case, it’s clear that the attack rate in Manaus is much higher than anywhere in the US or Europe, but this is not surprising if my theory is true.
Indeed, the population in Brazil is much younger than in the US or Europe, so although the attack rate climbed much faster over there, the numbers of deaths and hospitalizations have not. According to official statistics, as of December 8, 2020, 3,167 deaths had been attributed to COVID-19 for a population of approximately 2.2 million, which corresponds to a rate of about 1,438 deaths per million. By comparison, at this point, 11,593 deaths had been attributed to COVID-19 in Madrid. Since that city has a population of about 3.3 million, this corresponds to a death rate of approximately 3,470 per million. Thus, by December 8, the number of COVID-19 deaths per capita was actually higher in Madrid than in Manaus and presumably the same thing was true of the number of hospitalizations. However, even if you don’t buy that 75% of the population had already been infected by October in Manaus, the attack rate was no doubt much higher than in Madrid where seroprevalence was only ~11% in May and the vast majority of deaths were recorded before that. But if my theory is true, there is nothing surprising about that, since it’s only to be expected that it would take longer for people to change their behavior in a place where it takes longer for hospitalizations and deaths to start piling up because the population is younger. Thus, not only are such cases not counter-examples to my theory, but they’re actually predicted by it. I fully expect that, by the time the pandemic is over, we’ll find that the attack rate is higher in places with a younger population even controlling for various relevant variables.
Of course, as I have formulated it, this theory is very vague. In particular, I don’t give any precise figure to clarify what I mean by “rapidly diminishing marginal return” or “not very large effect”, but the truth is that I don’t think you can say anything more precise and people who claim otherwise are trying to fool you or are fooling themselves. I constantly see people on both sides of the debate throwing studies at each other that purport to estimate the effect of non-pharmaceutical interventions and allegedly prove that lockdowns and other stringent restrictions either work or don’t work. Those studies give very precise estimates of the effect of non-pharmaceutical interventions with confidence intervals that look very “scientific”, but all of that is completely meaningless because the models are poorly specified, the studies are plagued by omitted variable bias, measurement error, simultaneity, etc. Just remember how intractable it was to even figure out exactly when incidence started to fall in England, where there are much better data than virtually anywhere else in the world, then just imagine trying to disentangle causality in that mess with far noisier data. No wonder that you can find such inconsistent results in the literature on the effect of non-pharmaceutical interventions. In my opinion, the only studies that you may be able to take kind of seriously are those that use a quasi-natural experiment to estimate the effect of restrictions in a single country, such as this study on locally imposed lockdown in some Danish municipalities last November, which found no clear effect. But the conclusions of such studies can’t easily be generalized to other countries, so even they are not that useful.
However, I know that studies published in prestigious scientific journals exert a strong pull on people, so let me say more about the literature on the effect of non-pharmaceutical interventions. There are so many studies that claim to show that restrictions have a very strong effect on transmission, and so few people who have actually looked at them in detail, that I know people won’t take seriously my theory unless I do. In fact, when you take a close look at those studies, it becomes clear that none of them can possibly refute my theory and that all of them are completely unreliable if my theory is true. Most studies about the effect of non-pharmaceutical interventions fall roughly into 2 categories. First, you have studies that fit an epidemiological model, typically a compartmental model of some kind, on epidemic data. Non-pharmaceutical interventions are assumed by the model to affect transmission in a certain way and their effect is estimated by fitting the model. The other type of studies use econometric or machine-learning methods to estimate the association between non-pharmaceutical interventions and the growth rate of the epidemic or some related quantity such as .
The most famous example of the first type of study is probably Flaxman et al.’s paper that was published in Nature last June and has already been cited almost 750 times. This paper concluded that non-pharmaceutical interventions and lockdowns in particular had saved more than 3 million lives in Europe alone during the first wave and is still cited all the time by pro-lockdown advocates. I have already written a very detailed take-down of that study, which I strongly encourage you to read, so I’m not going to go over it again. To show how ridiculous the paper is, it suffices to say that, in order to obtain that estimate, the authors used a counterfactual in which more than 95% of the population had been infected by May 4 in every country they included in the study. Of course, even 9 months later, there is not a single country in the world as far as we know and certainly no country in Europe where the attack rate is even close to that. This is one of several little details the authors of that study decided not to state in the paper. The fact that such a preposterous estimate is still being taken seriously by so many people, including professional epidemiologists, tell you everything you need to know about how broken the scientific literature on the effect of non-pharmaceutical interventions is.
As I explain in my post about this study, their own results actually support my theory that, once a few very limited restrictions are in place, voluntary behavioral changes are enough to push below 1 long before the herd immunity threshold is reached. Indeed, they found that non-pharmaceutical interventions in Sweden, where there was no lockdown and restrictions were very liberal, had reduced transmission almost as much as in the rest of Europe. Nevertheless, they concluded that only lockdowns had a meaningful effect on transmission, because they included a country-specific effect in the model that allowed the effect of the last intervention to vary in each country. In every country besides Sweden, the last intervention was a lockdown and the country-specific effect is never very large, but in Sweden the last intervention was a ban on public events and the country-specific effect was gigantic. As I noted in my reply to Andrew Gelman’s comment about my post, the result was that while their model found that banning public events only reduced transmission by ~1.6% everywhere else, it found that it had reduced it by ~72.2% in Sweden, almost 45 times more. Of course, this never happened, there is just no way unless you believe Sweden is full of anti-covid magical fairies that banning public events was 45 times more effective in Sweden than anywhere else.
The fundamental problem with this paper is the same as with basically every other paper in that category I distinguished above and it’s that it assumes that only non-pharmaceutical interventions affect transmission. Thus, despite what people like the folks behind The Covid-19 FAQ continue to claim (even though I already explained to them why it was demonstrably false), there is no way studies of that sort could ever show that voluntary behavior changes wouldn’t push below 1 long before the herd immunity threshold is reached even in the absence of a lockdown, because they literally rely on models that implicit assume that voluntary behavior changes have no effect whatsoever on transmission. This is not just true of Flaxman et al.’s paper, but also of several other highly-cited studies, such as Brauner et al.’s paper in Science or more recently Knock et al.’s paper about the epidemic in England. Basically, what they do is assume that
or a related quantity such as the contact rate is affected by non-pharmaceutical interventions in a certain way, then fit the resulting model to the data to estimate the effect each of those interventions has. At best, what this kind of study can do is answer the question: if we assume that only non-pharmaceutical interventions affect transmission, and make a bunch of other largely arbitrary assumptions, what effect did each non-pharmaceutical intervention had on transmission? But we know that non-pharmaceutical interventions are not the only thing affecting transmission, so papers that follow this approach have no practical relevance whatsoever and predictions based on them are completely meaningless.
A second type of study doesn’t use an epidemiological model but tries to establish correlations between non-pharmaceutical interventions and the growth rate of the epidemic or some related quantity such as with traditional econometric or sometimes machine-learning methods. Basically, what they do is look at the epidemic in a bunch of different countries/regions and try to find if non-pharmaceutical interventions are associated with a reduction in the rate at which it grows, which is the case if the epidemic tends to grow less when non-pharmaceutical interventions are in place. The fundamental problem with this approach is that, if I’m right that people respond to epidemic conditions by modifying their behavior when hospitalizations and deaths start blowing up, then the epidemic’s growth rate will tend to start falling when the authorities decide to implement non-pharmaceutical interventions, because the people in charge also tend to do that when hospitalizations and deaths increase. So this kind of study would probably find a correlation between non-pharmaceutical interventions and a reduction of the epidemic’s growth rate even if the former didn’t have any effect on transmission, because the changes in epidemic conditions that make the authorities inclined to implement non-pharmaceutical interventions also make people change their behavior in ways that reduce transmission.
Similarly, it’s likely that if I gave you a pill that only contains sugar but told you that it’s a medicine that makes fever go down and you were the sort of person that only takes medicine when they’re at the point of death, you’d find that your temperature generally starts going down soon after you take it. But it would be wrong to conclude that it’s because the pill made your temperature go down. Indeed, we know the pill doesn’t do anything, it’s just sugar after all. The reason you’d probably find that your temperature usually goes down soon after you take the pill is that, since you’re the kind of person that only takes pill when they have already been in agony for days, by the time you finally take it, your immune system is mostly done fighting whatever caused the fever in the first place and your temperature was about to start falling anyway. This is what people call endogeneity when they want to sound intelligent, but as you can see, the basic idea is simple enough and anyone can understand it. I think it’s basically what happens with studies that look for correlations between non-pharmaceutical interventions and the epidemic’s growth rate. Again, I’m not saying that non-pharmaceutical interventions have no effect whatsoever, but they typically start around the time people start voluntarily changing their behavior, which hopefully I have convinced you probably has a very large effect on transmission. To be clear, it’s hardly the only problem with those studies, which among other things have to deal with massive measurement error and absolutely terrible data, but that alone makes the whole enterprise hopeless in my opinion.
A good example of this type of study is the paper by Haug et al. that was published in Nature back in November, which is one of the most sophisticated in the second category of studies. The authors used several different statistical approaches to estimate the relationship between non-pharmaceutical interventions and . Here is the figure that summarizes what they found:
 As you can see, if this study is to be believed, while some interventions are not effective, several of them have a large effect on transmission. Many people see that and conclude that it has been scientifically proven that restrictions had a very large effect on transmission, but as I already explained, this kind of study can’t establish causality and we have very good reasons to think their results are extremely misleading. What this means is that, if you use them to predict what is going to happen depending on what policy you implement, you will almost certainly get things catastrophically wrong. But it never occurs to people to check whether studies of that sort perform well out-of-sample, and reviewers apparently don’t ask their authors to do it, so they happily go around making policy recommendations based on papers that have essentially no practical relevance.
As you can see, if this study is to be believed, while some interventions are not effective, several of them have a large effect on transmission. Many people see that and conclude that it has been scientifically proven that restrictions had a very large effect on transmission, but as I already explained, this kind of study can’t establish causality and we have very good reasons to think their results are extremely misleading. What this means is that, if you use them to predict what is going to happen depending on what policy you implement, you will almost certainly get things catastrophically wrong. But it never occurs to people to check whether studies of that sort perform well out-of-sample, and reviewers apparently don’t ask their authors to do it, so they happily go around making policy recommendations based on papers that have essentially no practical relevance.
In the case of the Haug et al.’s paper, despite the fact that again it’s pretty sophisticated by the standards of that literature, you just have to eyeball a graph of in various US states during the past few months for 5 seconds to see that it performs horribly out-of-sample:
 I didn’t even bother to do this rigorously, but if you look up the restrictions in place in those states during that period and check Haug et al.’s paper, it’s obvious that we should have seen widely different trajectories of
I didn’t even bother to do this rigorously, but if you look up the restrictions in place in those states during that period and check Haug et al.’s paper, it’s obvious that we should have seen widely different trajectories of in those states and in particular that it should have been consistently much higher in states like Florida that remained almost completely open than in those like California that have put in place very stringent restrictions, but as you can see that’s not what happened. I only show a handful of states because otherwise the graph would be illegible, but I didn’t cherry-pick and, if you plot
in every state, you’ll see that it follows a very similar trajectory everywhere. You can do the same thing for Europe and you will reach the same conclusion.
Only a handful of studies make a serious attempt to address the endogeneity problem I have identified above. The best is probably the paper by Chernozhukov et al. about what happened in the US during the first wave that was recently published in the Journal of Econometrics, which as far as I know is the most sophisticated attempt to estimate the effects of lockdown policies in the literature. Indeed, unlike most papers in the literature about the effects of non-pharmaceutical interventions, it uses statistical methods that can in principle establish causality. The authors modeled the complex ways in which policy, behavior and the epidemic presumably interact. In particular, their model takes into account the fact that people voluntarily change their behavior in response to changes in epidemic conditions and that it’s typically around the same time that the authorities decide to implement non-pharmaceutical interventions, because they react to the same changes in epidemic conditions as the population, so if you’re not careful it’s easy to ascribe to non-pharmaceutical interventions what is really the effect of people’s voluntary behavior changes that would have occurred even in the absence of any government interventions. Again, it’s much better than most other studies I have read on the issue and the authors should be commended for at least trying to address the methodological problems I pointed out above, but I still don’t think you should buy their conclusions.
The effect sizes advertised in the abstract are pretty large but very imprecisely estimated and the rest of the paper shows that most of them are not robust to reasonable changes in the specification of the model. Their more robust finding is that mandating face masks for public-facing employees reduced the weekly growth in cases and deaths by more than 10%, which remains true in almost every specification of the model they tried, though not in all of them. Based on one of the specifications that was associated with the largest effect, they simulate a counterfactual in which face masks were nationally mandated for public-facing employees on March 14 and find that it would have reduced the cumulative number of COVID-19 deaths in the US by 34% during the first wave, but with a 90% confidence interval of 19%-47%. They are unable to estimate the effect of closing K-12 schools, but conclude that stay-at-home orders and the closure of non-essential businesses also reduced the number of cases and deaths, even though the effect is not significant in most of the specifications they tried. Even with the specification they used to define their counterfactual, they find that if no state had ordered the closure of non-essential businesses, the number of deaths would have been 40% higher by the end of May, but the 90% confidence is interval is extremely wide at 1%-97%. According to that same counterfactual, had no state issued a stay-at-home order, the number of deaths would have been somewhere between 7% lower and 50% higher.
Thus, even if you take their results at face value, I’d say this is hardly impressive. But I don’t think you should accept their results at face value, because as I plan to explain in a detailed post about this study, doing robustness checks in a more systematic way than the authors did reveals that, with the possible exception of the effect of mandating face masks for public-facing employees, everything in that paper is almost certainly just noise. Even the effect of mandating face masks for public-facing employees seems to be noise when you use weekly growth in cases instead of weekly growth in deaths as the outcome variable. Moreover, although the results when you use weekly growth in deaths are consistent with the effect being real, they are also consistent with the effect being spurious and I actually think that’s more likely, as I will argue in my forthcoming post about this study. It shouldn’t come as a surprise that even the most sophisticated pro-lockdown study falls short because, as we have seen, even a quick look at descriptive statistics is enough to convince oneself that, whatever the effect of non-pharmaceutical interventions, it can’t be huge, so any study that finds they have a massive effect is very unlikely to be correct.
Of course, as I already noted, there are also plenty of studies that find no or relatively modest effects of non-pharmaceutical interventions. (For instance, here is another study that attempts to disentangle the reduction of growth in cases that is due to policy from that due to voluntary behavior changes and finds that policy only explains 13% of the reduction in contact rate, whereas Chernozhukov et al. found that between 1/3 to 2/3 of the reduction in death growth could be attributed to policy depending on the specification of the model used.) However, they usually suffer from the same kind of methodological problems as pro-lockdown studies, so they can’t be taken seriously either. (There are many ways in which traditional econometric methods could go terribly wrong if they’re used to estimate the effect of non-pharmaceutical interventions. For more on that issue, see this paper, which goes over the problems that several widely used designs are likely to face in that context, as well as this paper, which uses simulations to show that most econometric methods used to estimate the effect of non-pharmaceutical interventions can easily produce very misleading results.) It doesn’t mean that all this confusion is completely uninformative though. On the contrary, like the fact that it’s impossible to detect any clear effect of non-pharmaceutical interventions by inspecting descriptive statistics, the fact that the literature on the effect of those interventions contains such inconsistent results is evidence that, whatever the real effect of non-pharmaceutical interventions, it’s not very large. Indeed, if non-pharmaceutical interventions had a very large effect, not only would it be easier to see it by inspecting descriptive statistics, but there probably wouldn’t be such a wide range of inconsistent results in the literature.
I think that, in that respect, the comparison with the impact of vaccination will speak volumes. I predict that, after a large enough share of the population has been vaccinated, not only will it be easy to see the effect by inspecting descriptive statistics, but the literature will consistently find that vaccination has a large effect. In fact, thanks to the fact that Israel has already vaccinated a large share of its population (including the vast majority of people over 60), we can already see that. Here is a graph from a recent paper that analyzed the data from Israel: This graph doesn’t involve any fancy statistical technique, it simply disaggregates based on age for a variety of outcomes, but the effect of vaccination couldn’t be clearer. Moreover, as the authors of that paper note, the same pattern wasn’t observed after the second lockdown, so we can be pretty confident this is the effect of vaccination.
This graph doesn’t involve any fancy statistical technique, it simply disaggregates based on age for a variety of outcomes, but the effect of vaccination couldn’t be clearer. Moreover, as the authors of that paper note, the same pattern wasn’t observed after the second lockdown, so we can be pretty confident this is the effect of vaccination.
Recent data from the US, where vaccination started in December, show a similar pattern: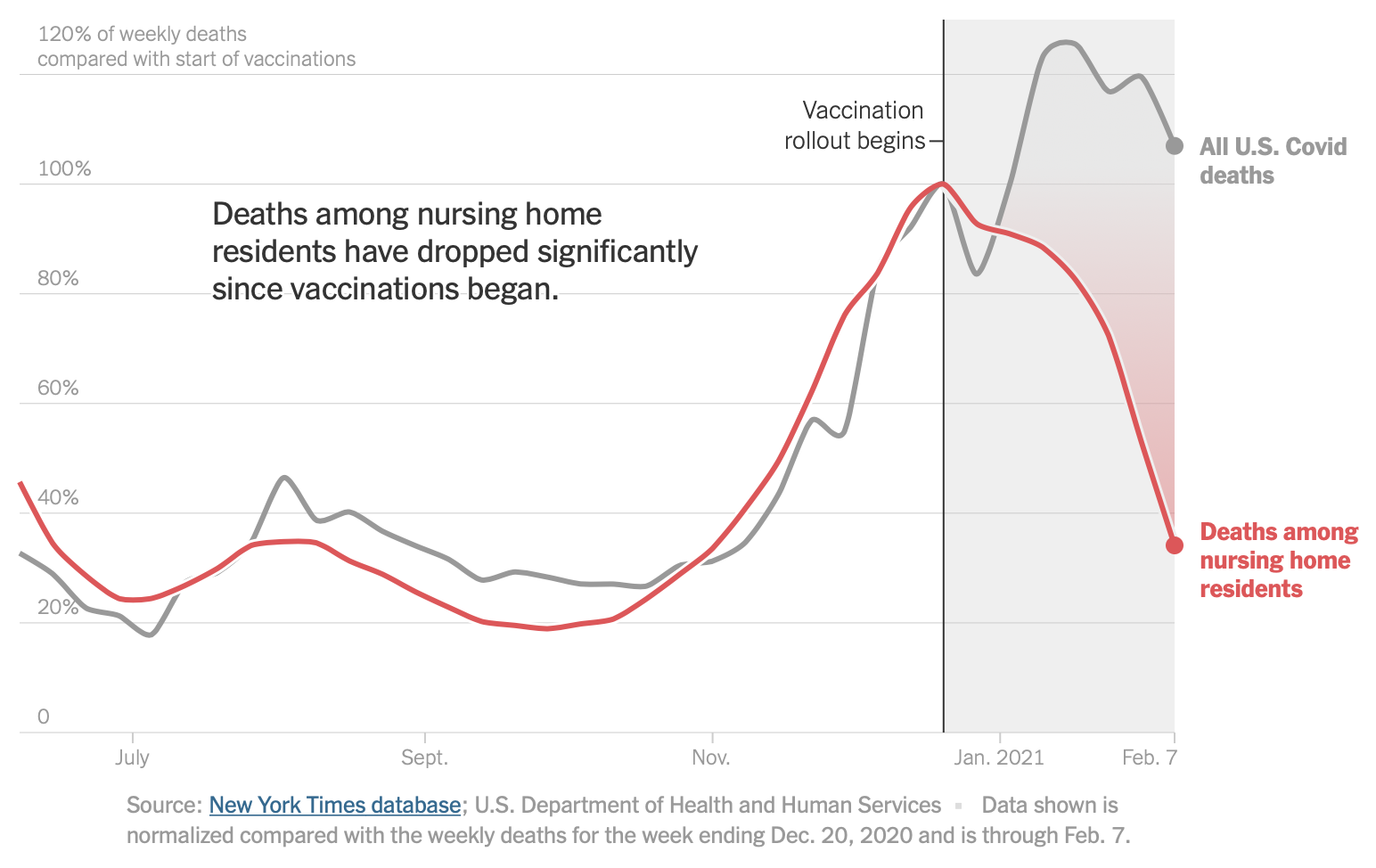 Now this is what a very large effect looks like and the contrast with non-pharmaceutical interventions couldn’t be more striking.
Now this is what a very large effect looks like and the contrast with non-pharmaceutical interventions couldn’t be more striking.
A question that often comes up when I present my theory is, if I’m right and most of the reduction in transmission results from voluntary behavior changes in response to changes in epidemic conditions, then how come everywhere the authorities are putting in place strict lockdowns and other stringent restrictions to reduce transmission. First, as I hope to have demonstrated, it’s simply false that governments are doing this everywhere. It’s just that, because of the bias in the way the media reports information about the pandemic, a lot of people don’t know that many places have eschewed the use of stringent restrictions for months and sometimes have never resorted to them at all. But I think I can also explain what’s happening in places where the authorities did put in place stringent restrictions. The epidemic quickly receded during the first wave after most places locked down, following China’s example in Wuhan, which convinced people that lockdowns were very effective because the post hoc ergo propter hoc fallacy is very natural. It did not matter that so-called “lockdowns” were far more relaxed in some places than in others and that it didn’t result in any obvious differences in the trajectory of the epidemic, let alone that incidence also declined quickly in Sweden where there was no lockdown at all. Moreover, for reasons I’m not going to speculate about, people really like to think that governments have control over the epidemic, so after the first wave the idea that any difference in outcomes had to be the result of policy differences quickly became received wisdom among commentators.
Now that it has become deeply ingrained in their minds, every time the epidemic starts blowing up again, the people in charge, who undoubtedly share that belief but are more reluctant to implement very stringent restrictions precisely because they are in charge and therefore perceive more clearly the social and economic consequences, find themselves under enormous pressure from the media to lock down. In most cases, they eventually give in, after which the epidemic starts to recede. As we have seen, this would also have happened even if there had been no lockdown and indeed that’s what happened in places that didn’t lock down, but it doesn’t matter because confirmation bias is a powerful drug. Post hoc ergo propter hoc! Again, the epidemic might have started to recede a bit later and it might have receded a bit more slowly, I’m not saying that lockdowns and stringent restrictions have no effect, but the difference would not have been huge and more importantly it wouldn’t have justified the cost of restrictions. Which brings me to the last topic I want to address in this post, namely how good lockdowns and other stringent restrictions look from a cost-benefit perspective.
Lockdowns and other stringent restrictions don’t pass a cost-benefit test
I don’t claim to be doing a rigorous cost-benefit analysis here. This is already a long post and, in order to be done properly, this exercise would require another, equally long post. But lockdowns and other stringent restrictions make so little sense from a cost-benefit perspective that I don’t even think it’s necessary, because a back-of-the-envelope calculation is sufficient to convince oneself that, unless one makes completely extravagant assumptions, their costs far outweigh their benefits. I will use Sweden as a case-study because it has become the standard-bearer of a more liberal mitigation policy, even though as we have seen many places, including some that locked down during the first wave, now have even fewer restrictions in place. However, after reading this, you should be able to easily do a similar back-of-the-envelope calculation about your own country or indeed any place you want. As we have seen, it looks as though Sweden might be at the beginning of a third wave, so if incidence continues to increase you can be certain that people both inside and outside the country will start clamoring for a lockdown. I’m going to argue that, despite what pro-lockdown advocates will say if this comes to pass, a lockdown or more stringent restrictions would make no sense from a cost-benefit perspective. In fact, it’s likely that Sweden should relax some restrictions, but in any case it should definitely not imitate countries like the UK, where a very strict lockdown has been in place since the beginning of the year. The same kind of calculation would show that countries such as the UK, where stringent restrictions are currently in place, should immediately start to lift them, because their costs far outweigh their benefits.
So far about 13,000 deaths have been attributed to COVID-19 in Sweden, though excess mortality since the beginning of the pandemic is a bit less than that. For the purpose of this cost-benefit analysis, I will assume that a lockdown in place for 2 months, followed by a gradual reopening over the next 2 months (similar to what the UK is doing), would save 15,000 lives during that period. To be clear, this assumption is completely absurd, no reasonable person should take it seriously. To give you a sense of how absurd it is, you just need to know that only ~13,000 deaths have been attributed to COVID-19 in Sweden during the past 12 months and excess mortality is actually less than that, so in effect I’m assuming that a lockdown would save more lives in 4 months than the total number of COVID-19 deaths since the beginning of the pandemic, even though Sweden never locked down. Moreover, although the process is absurdly slow as in the rest of the EU, vaccination has already started in Sweden and 80% of people in elderly care homes — where about half of COVID-19 deaths took place in 2020 — have already received their first shot, so we have every reason to believe that COVID-19 mortality will be considerably less in the months ahead even if as many people get infected as during the first wave, which is very unlikely given that the prevalence of immunity is much higher and that the population is no longer naive. As we have seen, it’s impossible to estimate precisely how many lives a lockdown would actually save, but there can be no doubt that it would be far less than that. Indeed, even if Sweden doesn’t lockdown, I would be amazed if there were half that number of COVID-19 deaths in the next 4 months, but a lockdown wouldn’t save all of them and it probably wouldn’t even save half of them.
People who die of COVID-19 tend to be very old and this seems to be even more true in Sweden than elsewhere. Indeed, as of February 21, 91.3% of people who died of COVID-19 in Sweden were 70 and over. In order to do a cost-benefit analysis, even a very rudimentary one as I’m trying to do here, we need to know how long the people who die of COVID-19 would have gone on to live if they hadn’t been infected by SARS-CoV-2. This recently published study estimates that COVID-19 victims lost on average 9.8 years of life in Sweden. (The authors don’t give that figure in the paper, but it’s easy to calculate based on table S3 in the supplementary information, which gives the number of COVID-19 deaths and the years of life lost per 100,000 by country.) However, this is at best an upper bound, because this estimate was obtained by assuming that people who died of COVID-19 had the same life expectancy conditional on their age and sex as people of the same age and sex in general. Of course, this is not true, people who die of COVID-19 tend to be in poorer health and their life expectancy conditional on age and sex is therefore lower. Thus, the actual number is no doubt significantly lower, though impossible to estimate precisely. Nevertheless, since I want to be as conservative as possible, I will assume that people who die of COVID-19 in Sweden lose on average 10 years of life. Combined with the ridiculous assumption I made about the number of lives a lockdown would save, I’m really stacking the deck in favor of lockdowns and other stringent restrictions. The assumptions I made so far imply that a lockdown would save 150,000 years of life in Sweden during the next 4 months, far more than the ~130,000 years of life that have been lost in that country in the past 12 months, under the same assumption about the average years of life lost by COVID-19 death.
It remains to discuss the costs that a lockdown would have during that period. When you talk about the costs of lockdowns and other stringent restrictions, people immediately think about the economic consequences. However, while I think the economic consequences of lockdowns and other stringent restrictions are likely to be significant in the long term (despite many ridiculous arguments to the contrary that would deserve another post), you don’t even have to consider them in order to convince yourself that such a policy doesn’t pass a cost-benefit test. So rather than making highly uncertain assumptions about the long-term economic consequences of lockdowns and other stringent restrictions, I’m only going to consider the immediate effect that restrictions have on people’s well-being. Indeed, while they are in place, restrictions reduce people’s well-being because they prevent them from doing many things they would like to do. Obviously, even in the absence of a lockdown, many people wouldn’t be able to live normally, but it would take a lot of bad faith to deny that, relative to life in Sweden under the current restrictions, life in the UK or even France where there is no lockdown but a curfew at 6pm and bars and restaurants have been closed since October really sucks.
One of the weirdest things about the cost-benefit debate on restrictions, beside the fact that it’s almost non-existent, is that almost everyone talks as if restrictions didn’t have an immediate effect on people’s well-being in addition to whatever economic consequences they have. Only a handful of cost-benefit analyses of COVID-19 restrictions have been published and, to my knowledge, not a single one of them has taken into account the contemporary effect of restrictions on people’s well-being. For instance, this recently published study whose authors conclude that a 4-week lockdown in February would have been cost-effective in the US only takes into account the short-term economic cost of such a policy, but totally ignores the immediate effect on people’s well-being. (She also makes the ridiculous assumption that, in the absence of a lockdown, the epidemic would continue its course as predicted by a SIR model with constant contact rate that includes vaccination, while a lockdown would immediately push to 0.62. This is the kind of nonsense people are talking about when they claim that lockdowns and other stringent restrictions are scientifically proven means of fighting the pandemic.) What I want to do is compute the upper bound of the immediate effect a lockdown would have on people’s well-being in order for the benefits of that policy to outweigh the cost.
This is a very straightforward calculation and you could easily do the same thing for other places. In the case of Sweden, since we have assumed that a 2-month lockdown followed by a gradual reopening over another period of 2 months would save 150,000 years of life over 4 months and Sweden has a population of 10.2 million, a lockdown would have to reduce people’s well-being by at most 150,000 / (10,200,000 * 4 / 12) = 4.5%. In other words, you would have to assume that, in exchange for not being locked down in the way people in the UK currently are but instead living under the same kind of restrictions they currently are (i. e. being able to go to a bar or a restaurant even if the sale of alcohol is prohibited after 8pm, to meet anyone they want whenever they want, to put their children under 16 in school, to go to the gym, see their colleagues at least some of the time, etc.), people would not be willing to lose about 5 days and a half during the next 4 months. It would be kind of tricky to elicit people’s preferences on the subject, though it shouldn’t be impossible. On the one hand, you’d have to make sure their answer doesn’t take into account their preferences for reducing the spread of the virus, because we’re asking them in order to estimate what impact a lockdown would have on their well-being independently of what they expect the benefits of that policy to be on reducing the spread. Indeed, we are already taking into account the expected benefits of a lockdown on transmission, so doing that would amount to a form of double counting. On the other hand, we can’t ask them to imagine there is no pandemic when they answer the question, because there is a pandemic and it means that people wouldn’t be able to benefit from their freedom as much as usual.
Nevertheless, I have no doubt that on average people would be willing to sacrifice more than 5 days and a half during the next 4 months to enjoy that kind of freedom, rather than live under the kind of restrictions people in the UK have to deal with. Moreover, keep in mind that, in order to estimate this upper bound of the reduction of well-being caused by a lockdown, I have made preposterous assumptions about how many years of life a lockdown would have. If we assume that a lockdown would only save 5,000 lives and that the average years of life lost per COVID-19 death is 7.5 years, which in my opinion are still overestimates (5,000 is approximately the total number of deaths in Sweden during the first wave, when the population was behaviorally naive, nobody had acquired immunity through natural infection and vaccination was not ongoing), it would have to be the case that a lockdown would at most reduce people’s well-being by ~1.1% on average over the next 4 months. In other words, for a lockdown to pass a cost-benefit test under those assumptions, you’d have to assume that on average people in Sweden would not be willing to sacrifice more than ~32 hours in the next 4 months to continue to live the semi-normal life they currently enjoy instead of being locked down. Given my lifestyle, I’m pretty sure that I’m one of the people who has the least hard time dealing with restrictions, but even I would sacrifice more than that. This is just absurd and I would have a hard time believing that someone who insists this actually makes sense is arguing in good faith.
If you assume that, compared to the current level of restrictions in Sweden, a British-style lockdown would reduce people’s well-being by 10% on average over a period of 4 months and make the more reasonable though still unrealistic assumptions I just made about the number of years of life that a lockdown would save, it follows that its costs would exceed its benefits by a factor of 9. Of course, this cost-benefit analysis is little more than a back-of-the envelope calculation, but I think the results are so lopsided that it’s more than enough to convince oneself that even a rigorous cost-benefit analysis would not vindicate lockdowns and other stringent restrictions. It’s true that, on the costs side of the ledger, I have only taken into account years of life lost. But the virus has costs even for people who survive infection, especially those who developed a severe form of the illness. But despite the hysteria about “long COVID”, if you make realistic hypotheses, the consequences for survivors are only going to be second-order effects relative to the years of life lost by the people who died. (There would be a lot to say about the literature on “long COVID”, which makes the literature on the effect of non-pharmaceutical interventions look like the pinnacle of science, but I guess it will be for another time.) For instance, in Sweden, only 5,252 people had been admitted to ICU for COVID-19 as of February 24. Even if you assume that it reduced their well-being by 50% for a whole year, the equivalent in years of life lost is only ~3% of the years of life lost by the people who died of COVID-19 since the beginning of the pandemic when you assume 7.5 years of life lost by COVID-19 death, which is negligible.
But I have also ignored a lot of things on the costs side of the ledger, since I have only taken into account the immediate effect of restrictions on people’s well-being, which most people don’t even think about when they talk about the cost-benefit aspect of the debate on lockdowns and other stringent restrictions. In fact, I have no doubt that the economic consequences of lockdowns alone dwarf the effects of COVID-19 on people who survive, despite the ridiculous slogan that “lockdowns don’t destroy the economy, the virus does”, which is constantly recited like a mantra by pro-lockdown advocates. It would take a whole post to properly address the issue, which I may write eventually, so I will just point out that while obviously the virus alone is doing a lot of damage to the economy, it’s very silly to deny that restrictions also don’t have a large effect. In fact, even the handful of cost-benefit analyses of lockdowns that have been published, such as the one I mentioned above, assume that lockdowns have a large economic cost. People commit all sorts of fallacies when they talk about this, such as making international GDP comparison based on data that can’t be compared, citing a study that only used data on the first wave to draw conclusions about what should be done now even though the effect of the pandemic on behavior became starkly different after that or using a study that compared Sweden to other Scandinavian countries, where lockdowns were relatively mild and short compared to the rest of Europe, to conclude that very strict lockdowns would not do much economic damage above and beyond what the pandemic itself would cause.
But the central problem seems to be that people who claim there is no trade-off between economic and health outcomes don’t seem to understand that whether it’s true crucially depends on the context. If you have managed to bring incidence down to a very low level and that you can keep it there, as some countries have somehow managed to do, then it’s probably true that doing so is the best way to protect both people’s health and the economy. But this fact is completely irrelevant when arguing that countries such as Sweden, France or the US should lock down now, because the reality is that unlike the countries cited in example by the people who claim there is no trade-off between economic and health outcomes, they have not managed to keep incidence low and it’s currently very high in all of them. But when incidence is high, there is no question that bringing it down is very costly, so the fact that localized, short lockdowns whenever a cluster appears somewhere might be the optimal policy when you have managed to suppress the virus is completely beside the point. It’s a bit as if people had told Hitler in April 1945 that, in order to repel the Soviet attack, the best strategy would be to throw 50 armored divisions at Zhukov’s army. Well, sure, this sounds like a great idea, except for the fact that by then Hitler didn’t have any armored division, let alone 50 of them, to throw at Zhukov. So while this argument about the absence of a health-economy trade-off might have been convincing in Europe last Summer, when incidence was very low, it’s completely irrelevant now. In fact, I don’t even think it would have been convincing then, because I don’t think Europe or the US could plausibly have managed to keep incidence very low, but I’ll discuss this below.
In addition to the effect they have on the economy, I have ignored many other costs of lockdowns. For instance, data recently came out in France about cancer diagnoses, which show they have fallen by more than 23% in 2020 compared to the previous year. Of course, not all of the people who failed to get diagnosed in time will die and for some being diagnosed in time would not have prolonged their life much, but we’re still talking about ~93,000 missing diagnoses and it seems that it could result in between 3,000 and 24,000 excess deaths in the years to come. However, not only is it difficult to estimate what this means in terms of years of life lost, but presumably not all of those missing diagnoses are due to lockdowns. In Italy, recently published data show that the lethality of heart attack, which is a major cause of death, tripled in 2020. Again, some of that increase would no doubt have occurred even in the absence of a lockdown and it’s difficult to estimate how many years of life were lost because of that, but surely lockdowns caused some deaths. On the other hand, they probably reduced the number of deaths for some other causes, such as traffic accident fatalities, although we’re talking about pretty small numbers. Lockdowns and other restrictions may also have prevented deaths caused by other respiratory viruses, though just as for the effect of the spread of SARS-CoV-2, it’s hard to disentangle what is due to non-pharmaceutical interventions and what is due to voluntary behavior changes. My guess is that, setting aside COVID-19 deaths, lockdowns actually caused some excess deaths, but I have no doubt that all of that is dwarfed by the years of life lost because of COVID-19 deaths.
Once you take into account COVID-19 deaths and the effect lockdowns and other stringent restrictions had on them, their effect on mortality is almost certainly positive (i. e. they reduced excess mortality), but as I have argued above it’s nowhere as large as pro-lockdown advocates claim and the effect they have on people’s well-being alone is enough to make them completely irrational from a cost-benefit perspective. Again, this is true even when you ignore the economic consequences of restrictions, which likely dwarves every other thing I didn’t take into account. If you think I’m wrong, it’s not enough to say that you disagree with any particular assumption I have made, you have to show that, had I made other assumptions that you consider more plausible, the conclusion would have been different. Honestly, I don’t believe for a moment that it’s possible without making completely unrealistic assumptions, but you can always try. The truth is that I’m not even sure that lockdowns and other stringent restrictions would pass a cost-benefit if you ignored everything I said in the first part of this essay and assumed that, in the absence of a lockdown, incidence would increase quasi-exponentially until the herd immunity threshold is reached in a few weeks. But it doesn’t really matter because, even though many people continue to insist this is true, the evidence against this claim is completely overwhelming and making it today should be disqualifying. Moreover, it’s important to note that, despite what many people claimed when preliminary results showing the vaccines are highly effective were announced, the availability of vaccines didn’t change the fact that lockdowns and other stringent restrictions don’t pass a cost-benefit test. Indeed, nowhere in my argument do I assume that, if the costs outweigh the benefits, it’s because restrictions only save lives temporarily because they merely delay the inevitable. Stringent restrictions didn’t pass a cost-benefit test before we knew that vaccines would soon be available and still didn’t after we learned that for sure.
I know that many people who find the principle of such a cost-benefit analysis itself absurd on the grounds that “even a single life has no price”, but this is just a slogan and nobody really believes that. To convince you of this, imagine that a demon told us that, unless we agree to lock down the entire world for 10 years, he will kill one person at random. It’s obvious that no one but a handful of lunatics would accept this deal. Of course, if the demon told us that he was going to kill more people or that in order to avoid this we wouldn’t have to agree to lock down the entire world but only some parts of it and for less than 10 years, then depending on the details you might determine that it would be worth it. But this thought experiment shows that, even if you are one of those people who say that “even a single life has no price”, you don’t really believe that when you say it. There comes a point when the cost becomes large enough that you are willing to sacrifice lives. If this weren’t the case, life would be impossible because everything, including the most trivial activities, has a non-zero risk for you and others. Once you accept this principle, you accept the logic of a cost-benefit analysis. Of course, no one is saying that it’s easy to carry out, that’s a separate question. On the contrary, everybody who is familiar with that exercise knows that it’s very difficult to do properly. But that doesn’t mean you shouldn’t try, if only because it forces you to ask yourself what assumptions you are making to guide your decisions, which can prevent you from making a huge mistake.
With the beginning of the vaccine rollout, you would have thought that calls to lock down would subside. In fact, back in the Fall (after it became clear that vaccines would soon be available), that’s exactly what pro-lockdown advocates used to say in order to sell restrictions. They were saying that, now that we knew for sure that vaccines would soon be available, lockdowns were more warranted than ever because vaccines would soon make them redundant, so we just had to hang in there and bear the restrictions for a few extra months before we could finally lift them. But instead the same people are now calling for even more restrictions and a so-called “zero COVID” strategy, which consists in bringing incidence to a low enough level with a strict lockdown, at which point most restrictions can be lifted safely and people resume a normal life because contact tracing will be able to keep it there. To be honest, I really think that some people have basically developed a bizarre addiction to restrictions at this point and that as a result they will seize any rationale to push for more of them, but nevertheless I want to discuss this so-called “zero COVID” strategy because it has become very popular among the educated class even though I think it’s completely nonsensical.
It’s very difficult to talk about the “zero COVID” strategy because, like “abolish the police”, it’s more a political slogan than a well-defined policy, so its proponents are often vague and they often don’t say the same thing. Although the lines of reasoning are not always clear, as far as I can tell, at least 3 distinct arguments in favor of a “zero COVID” strategy can be reconstructed:
- Even putting aside the threat posed by new variants, either those that have already emerged or those that might emerge if SARS-CoV-2 continues to circulate a lot, bringing incidence back to a very low level with a lockdown and using contact tracing to keep it there is optimal from a cost-benefit perspective because, as countries such as Australia and New Zealand showed, it’s the best way to lift restrictions and resume a normal life quickly instead of the “stop and go” policy that most Western countries have adopted.
- Because new variants such as B.1.1.7 are more transmissible, a lockdown would give us time to increase the prevalence of immunity in the population by vaccinating as many people as possible, so that when restrictions are lifted the higher
will not matter because it will have been “canceled” by the higher prevalence of immunity. Even if vaccines turn out not to protect against infections by the new variants, it won’t matter because the most at-risk people will have been vaccinated and this will at least protect them against severe forms of the illness.
- The more SARS-CoV-2 circulates, the more likely it is that new variants will emerge that evade both the immunity induced by vaccination or by natural infection with the wild type of the virus, which would bring us back to square one. By reducing circulation of the virus, a lockdown followed by contact tracing to keep incidence low will prevent such a variant from emerging and we won’t lose the benefits of all the efforts we have made so far because a new variant causes what would effectively be a new pandemic.
Those lines of reasoning are often run together by proponents of the “zero COVID” strategy, but they are distinct arguments, so I think it’s important to distinguish them. Moreover, although they are not mutually exclusive, their premises are sometimes in tension.
I will start the first argument, which predates the emergence of B.1.1.7 and the other variants that people now worry about. As I just explained, according to the proponents of the “zero COVID” strategy, the first step of that strategy consists of implementing a strict lockdown to bring incidence down to a low enough level. They claim that, with a strict lockdown, this could be done quickly. While they are careful not to commit to any specific duration in their platform, such as this statement published in several large European newspapers and signed by many scientists, they often talk about a 4-week lockdown. There reasoning seems to be that, even if you start from a relatively high level of incidence like 20,000 cases by day (which corresponds roughly to the plateau in France since the beginning of the year), assuming the generation time distribution has a mean of 4 days, a lockdown that pushes down to 0.7 would bring incidence back to less than 2,000 cases by day in a month. At this point, still according to the proponents of the “zero COVID” strategy, contact tracing could prevent another explosion and keep incidence low, which at 20,000 cases by day is simply not possible because the number of contacts to trace would be ridiculous. This looks pretty convincing in theory, but in practice things are more complicated. I’ll go back to contact tracing later and whether it could really do what the proponents of that strategy think, but first I want to discuss the reasoning they use to argue that a short lockdown would be enough to bring incidence back to a level where contact tracing can realistically work.
The best way to see that reality doesn’t usually cooperate with that kind of simplistic calculations is to look at some examples and what better example than Australia, which the proponents of the “zero COVID” strategy like to mention every chance they get? On July 9, as incidence had been increasing again, the state of Victoria placed Melbourne on lockdown for what was supposed to be a period of 6 weeks. But here is what actually happened: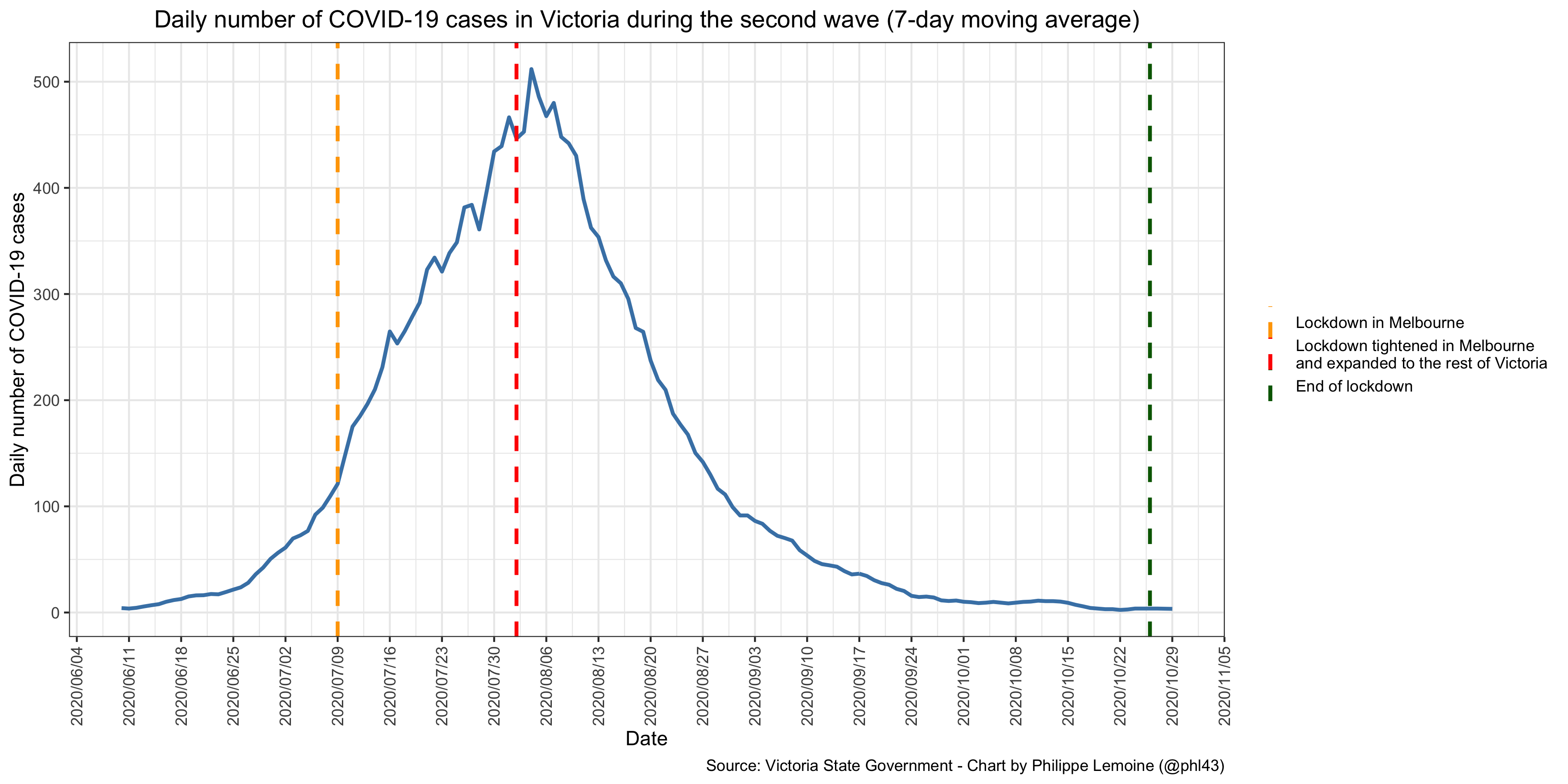 As you can see, despite the lockdown that was ordered in Melbourne at the beginning of July, incidence continued to rise for almost a month, which is yet more evidence for my theory that lockdowns aren’t always sufficient to push
As you can see, despite the lockdown that was ordered in Melbourne at the beginning of July, incidence continued to rise for almost a month, which is yet more evidence for my theory that lockdowns aren’t always sufficient to push below 1 because what’s really driving transmission is people’s behavior and restrictions are not very good at targeting the kind of behaviors that contribute the most to transmission. On August 2, the rules of the lockdown were tightened in Melbourne, while the rules previously in place in Melbourne were extended to the rest of the state. Pro-lockdown advocates claim that incidence fell as a result of that, but since incidence seems to have peaked sometime between July 29 and August 4, once you take into account the incubation period it’s likely that
fell below 1 before the rules were tightened. In the end, the lockdown lasted 109 days in Melbourne, even though it was originally supposed to last only 6 weeks. Even if you buy the pro-lockdown argument that it wasn’t really a lockdown until the rules were tightened on August 2 and assume that it could have been ended safely on October 1, that’s still twice as long as the 4-week that proponents of the “zero COVID” strategy are trying to sell us. Yet even at the peak of the second wave, incidence in Victoria was only ~1/4 of that in France at the beginning of the year. I could have made the same point with the example of Wuhan, where the lockdown lasted 76 days, despite being far stricter than anything that could realistically be done in the West, especially after almost a year of restrictions.
The problem with the nice little calculation that proponents of the “zero COVID” strategy make is that, even if they don’t realize it, they make a lot of assumptions that are simply not plausible. In particular, it assumes that as long as the same restrictions in place will remain the same and in particular that it doesn’t depend on incidence, so that if a strict lockdown can bring it to 0.7 it will stay there for the whole duration of the lockdown. But in practice that’s never what happens and, if my theory is correct, there is nothing surprising about this. Again, what really drives transmission is people’s behavior and it responds to change in epidemic conditions, so when incidence falls they eventually relax and
starts rising again even if the restrictions in place are exactly the same, because restrictions only have a limited effect on the behaviors that affect transmission the most and people’s voluntary behavior matters more. (Indeed, if you look at mobility data for the UK below, you will see that mobility started to fall before the third national lockdown and that after reaching a trough it has been going up since then despite no relaxation of the rules.) Another implicit assumption of the calculation that proponents of the “zero COVID” strategy make to argue that a 4-week lockdown would be sufficient is that the generation interval will remain the same, but to the extent that a lockdown works, it’s conceivable that it could lengthen the generation interval. However, even keeping
equal, a longer generation interval results in a higher rate of growth, in which case it will also take longer than anticipated to bring incidence down to the same level. Thus, despite the simplistic calculations advertised by proponents of the “zero COVID” strategy, there is no doubt that in places where incidence is currently high it would take more than 4 weeks of lockdown to bring it back to a low enough level for contact tracing to take over.
Not only would it be harder for the US or European countries to replicate what Australia and New Zealand did because in most of them incidence is currently higher than it ever was in Australia and New Zealand, but it would also be more difficult because they are far less isolated from the rest of the world. In particular, European countries are strongly integrated with each other, with a lot of people traveling between them for economic, cultural and other reasons. Obviously, this is even more true of the US, where a lot of people travel between states. First, they would have to close their borders to each other for a long time, which given how integrated they are would have a much higher economic and human cost than in Australia and New Zealand. This couldn’t realistically last very long, but unless they all managed to suppress the virus, the virus would start to spread again as soon as they opened their borders to each other, so they would have to coordinate to implement this strategy more or less simultaneously even though the epidemic doesn’t follow the same course at the same time everywhere. I know that proponents of the “zero COVID” strategy have imagined putting in place zones between countries that have managed to suppress the virus, within which people could travel more or less freely, but even that would require a lot of coordination. This coordination problem alone, that Australia and New Zealand never had to face (which is why I think Europe couldn’t have pulled off what Australia and New Zealand did even last Summer when incidence was very low everywhere), is sufficient to make the whole project completely unrealistic, yet as we have seen it’s hardly the only obstacle. It’s the sort of nonsense that people who are totally removed from political decision-making come up with because they ignore the economic and political constraints that decision-makers face, but you just can’t wish those constraints away.
Even if all countries in Europe and states in the US somehow managed to more or less simultaneously bring incidence back to a very low level, they would have to keep it low after that. The proponents of the “zero COVID” strategy are counting on contact tracing to do the job, but it’s doubtful that it would actually work. First, it has never worked in the past to prevent another explosion of incidence anywhere in Europe or the US, so it doesn’t seem very reasonable to count on it to work the next time. You may think that it’s because we didn’t do it right before, so it doesn’t mean that it wouldn’t work if we tried again, but what makes you think that governments that have failed to implement contact tracing correctly in the past will succeed now? I’m sure you’ve heard the quote attributed to Einstein about the definition of insanity and, while I think he never actually said that, I still think it applies pretty well here. The proponents of the “zero COVID” strategy are asking that we implement a very costly lockdown, especially since as we have seen it would last much longer than they claim and may not even be enough to bring incidence where they think it would need to be in order for contact tracing to work, on the assumption that the health authorities would do better than before. I don’t know about you, but if there is one thing this pandemic didn’t do, it’s increase my confidence in the ability of the people in charge to learn from their mistakes. It’s all the more unlikely in the case that, if as the proponents of the “zero COVID” strategy insist, B.1.1.7 is really more transmissible than the wild type, which would also make contact tracing more difficult. Strangely, despite their obsession with the new variants, the proponents of that strategy apparently did not think about that.
But frankly I’m not even convinced that, if contact tracing wasn’t able to prevent incidence from exploding in the past, even in Europe last summer when incidence was very low everywhere, it’s because it was done poorly rather than because it was intrinsically very difficult to pull off. The proponents of the “zero COVID” strategy just assume that is the case, but the truth is that nobody knows. Similarly, they claim that, if most East Asian countries were able to keep incidence low, it’s because of contact tracing, but they actually have no idea. Indeed, they used to say the same thing about Germany, but we know what happened next. All they know is that most East Asian countries were able to keep incidence low without locking down and that they used some kind of contact tracing, but they don’t know that it’s because of contact tracing and in some cases I actually find that hypothesis extremely implausible. If you want to say that rich countries such as South Korea, with a well-funded health care system and high quality infrastructure, were able to keep incidence low thanks to contact tracing, that’s something I can believe. But if you tell me that’s the reason why countries such as Cambodia, Myanmar and Thailand, which have a GDP per capita that are respectively ~1/29, ~1/33 and 1/6 that of Germany, were able to contain the pandemic without lockdowns, then I don’t know what to say other than you urgently need to come back to reality. I don’t know why East Asian countries were largely spared by the pandemic, but whatever the explanation, I know that it can’t be just because of their awesome contact tracing. The fact that such a ridiculous idea has become received wisdom speaks volumes about the state of public discourse. The truth is that, compared to Western countries, many of those places did almost nothing to stop the spread of SARS-CoV-2 but were vastly more successful, so clearly there must be other factors.
Incidentally, note that Australia and New Zealand, despite having vastly more resources than Cambodia, Myanmar and Thailand, don’t trust that contact tracing alone can keep incidence low since they now lock down entire cities as soon as a few cases are detected. To be clear, I do not doubt that contact tracing can reduce transmission, but the truth is that we have very little evidence about the effect it has. As far as I know, the best we have is a very ingenious study that exploited quasi-random variation in contact tracing in England due to a data processing error (it turns out that Excel is actually good at something, even if that’s because it’s bad), but while I think it’s good evidence that contact tracing can reduce transmission and save lives, it’s hard to generalize the results beyond England and there is no way to conclude from this paper that contact tracing would be enough to keep incidence low for several months after a lockdown even in England. It’s possible that, were it not for cultural and legal constraints that limit how intrusive contact tracing can be in Western countries, it could actually keep incidence low after a lockdown. Perhaps contact tracing is actually what allowed South Korea to contain the pandemic because it didn’t face those constraints, but again we don’t actually know that and, in any case, the fact is that Western countries do face those constraints, so it wouldn’t do them any good even if that were true.
Moreover, unless the proponents of the “zero COVID” strategy propose that European countries and US states keep their borders closed to each other even after incidence has fallen to a very low level until almost everyone has been vaccinated (which in the EU at least will probably not happen until this summer at the earliest), a failure in any country or state would endanger all the others. Even if the other countries or states put the one where contact tracing failed in quarantine as soon as incidence started increasing again, given the lag between the time infections start to increase and the time it shows up in the data about tests, the exponential nature of the process in the short-run and how integrated European countries or US states are, there is a serious risk that a resurgence of the pandemic in one of them would quickly spread to the others, which may actually be part of the explanation why Europe and the US had a harder time keeping incidence low. Beside, this would also require a lot of coordination, which as we have seen would be very difficult if only for political reasons. In short, given the situation in Europe and the US at the moment, the “zero COVID” strategy is a fantasy that will never happen. Even if that were a realistic option, you could easily show by the same argument as before that it would make no sense from a cost-benefit perspective, especially since as I argue it would take a lot more than 4 weeks to reach a point where it’s safe to lift restrictions. Again, the “stop and go” policy that most Western countries are currently using is entirely self-imposed, they could lift most restrictions immediately and it would be a clearly superior option from a cost-benefit perspective. Moreover, since most at-risk people will soon have been vaccinated even in the EU (where the process is excruciatingly slow), the cost of the pandemic is about to fall dramatically, which brings me to the second argument in favor of the “zero COVID” strategy.
The argument is that, since B.1.1.7 is significantly more transmissible than the wild type and it will soon be dominant everywhere in Europe and the US, it makes sense to lock down to prevent incidence from exploding. Note that it doesn’t even follow from this argument that we should keep incidence low indefinitely but only long enough for us to vaccinate enough at-risk people, though of course if we can keep it low with contact tracing it’s even better as long as it’s not too expensive. In fact, it doesn’t even imply that incidence be pushed very low, just that it be prevented from exploding due to the more transmissible new variants. Presumably, in order to calculate the optimal number of at-risk people that should be vaccinated before restrictions are lifted, a cost-benefit analysis would have to be carried out to balance the cost of the lockdown needed to prevent incidence from exploding because of the new variants. The problem with that argument is that it assumes that lockdowns are extremely effective to reduce transmission and make a huge difference relative to a situation where few restrictions are in place but people voluntarily change their behavior in response to changes in epidemic conditions, but as we have seen the evidence doesn’t support that view. If the variants really were incredibly more transmissible than the wild type, this might still make sense, because even the modest difference that lockdowns and other stringent restrictions probably make could be what it takes to push below 1. But I think at this point it’s perfectly clear that, despite what people initially thought and what many continue to think, the extent to which B.1.1.7 is more transmissible than the wild type has been wildly overestimated. There is clearly something different about that variant, but I don’t see how people can still maintain that it’s 70% or even 50% more transmissible than the wild type.
There are several ways to convince oneself of that. One of them is to look at epidemic data in places where B.1.1.7 has recently been spreading. For instance, according to the French government, the prevalence of B.1.1.7 was ~3.3% on January 8 and ~39.5% or ~49% during the week between February 15 and February 21, depending on whether you use full-sequencing data or data based on S-gene target failure after a PCR or antigen test. Yet here is how incidence, , and mobility have changed between January 8 and February 21:
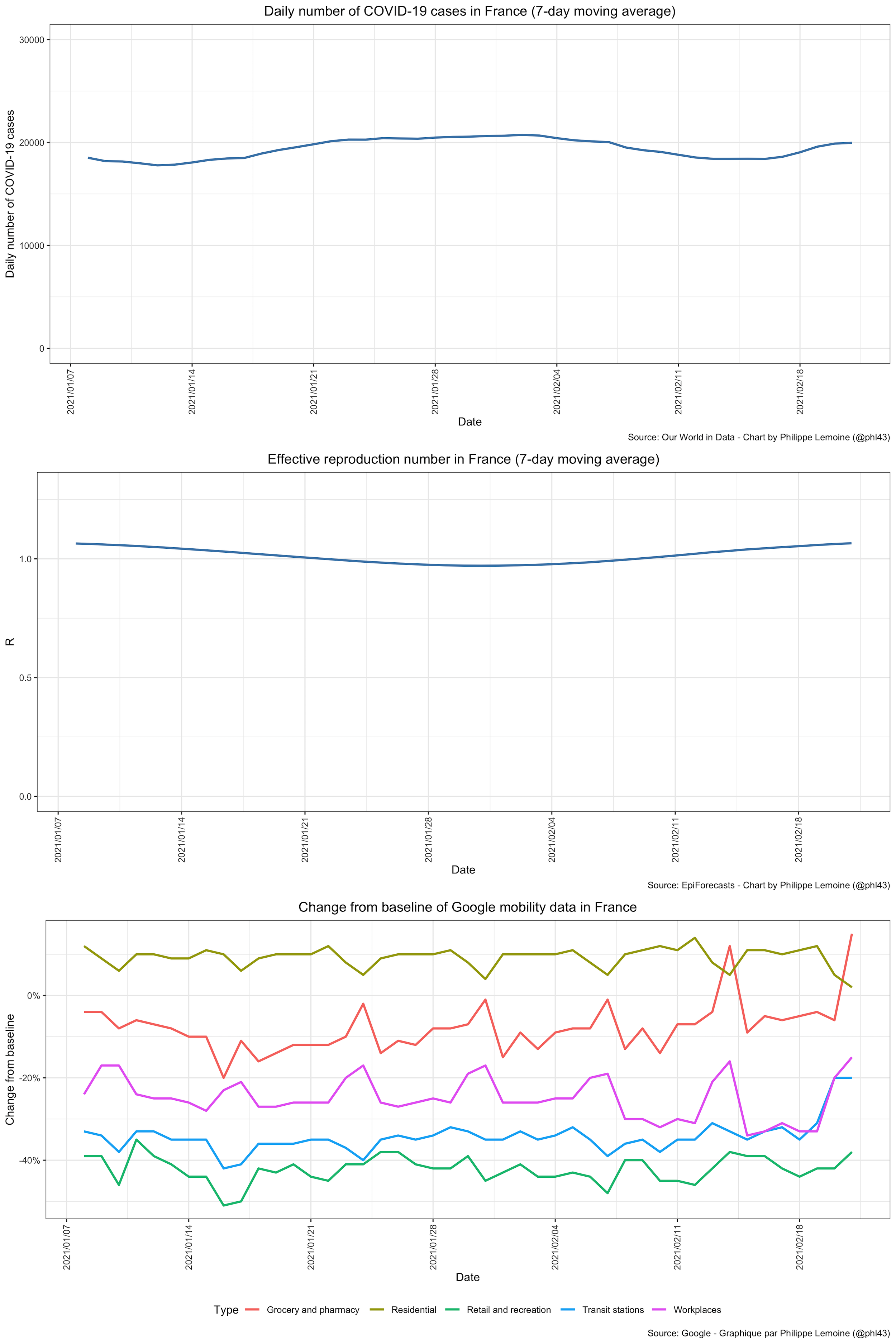 Incidence recently started increasing again in France, but we don’t have data on the prevalence of B.1.1.7 after week 7, so I only show the data up to February 21.
Incidence recently started increasing again in France, but we don’t have data on the prevalence of B.1.1.7 after week 7, so I only show the data up to February 21.
As you can see, everything was basically flat during that period. If you infer effective reproduction numbers in the straightforward way from the data on incidence and the prevalence of B.1.1.7 among positive samples, depending on what assumptions you make about the generation time and whether you use full-sequencing data or data based on S-gene target failure, you find that it’s between 30% and 45% more transmissible than the wild type. However, for that inference to be correct, it would have to be the case that has gone down significantly for the wild type during that period even though mobility was completely flat. Now, I know the data about everything are extremely low quality here and we must therefore be careful in drawing conclusions from them (in particular I think there are good reasons to think that mobility data are a very noisy measure of the behaviors that drive transmission), but I would be surprised if B.1.1.7 was more than 30% more transmissible than the wild type and I don’t see how it could be 70% more transmissible or even 50% more transmissible.
Indeed, when epidemiologists made short-term projections based on the assumption that B.1.1.7 was more transmissible than the wild type to such a large extent, they failed miserably everywhere. For instance, here is a projection made on January 29 by the Scientific Council, which advises the French government about the pandemic, based on the assumption that B.1.1.7 was 50% more transmissible than the wild type: As you can see, both incidence and hospital admissions were supposed to start increasing exponentially at the beginning of February (you will also note that the epidemiologists who advise the French government continue to assume that people don’t voluntarily change their behavior when incidence explodes), but as we have seen it actually decreased in February until it started increasing again recently.
As you can see, both incidence and hospital admissions were supposed to start increasing exponentially at the beginning of February (you will also note that the epidemiologists who advise the French government continue to assume that people don’t voluntarily change their behavior when incidence explodes), but as we have seen it actually decreased in February until it started increasing again recently.
Another way to see that, no matter how transmissible B.1.1.7 is, the difference with the wild type can’t be as large as originally claimed is to look at curves of incidence in places where it’s dominant: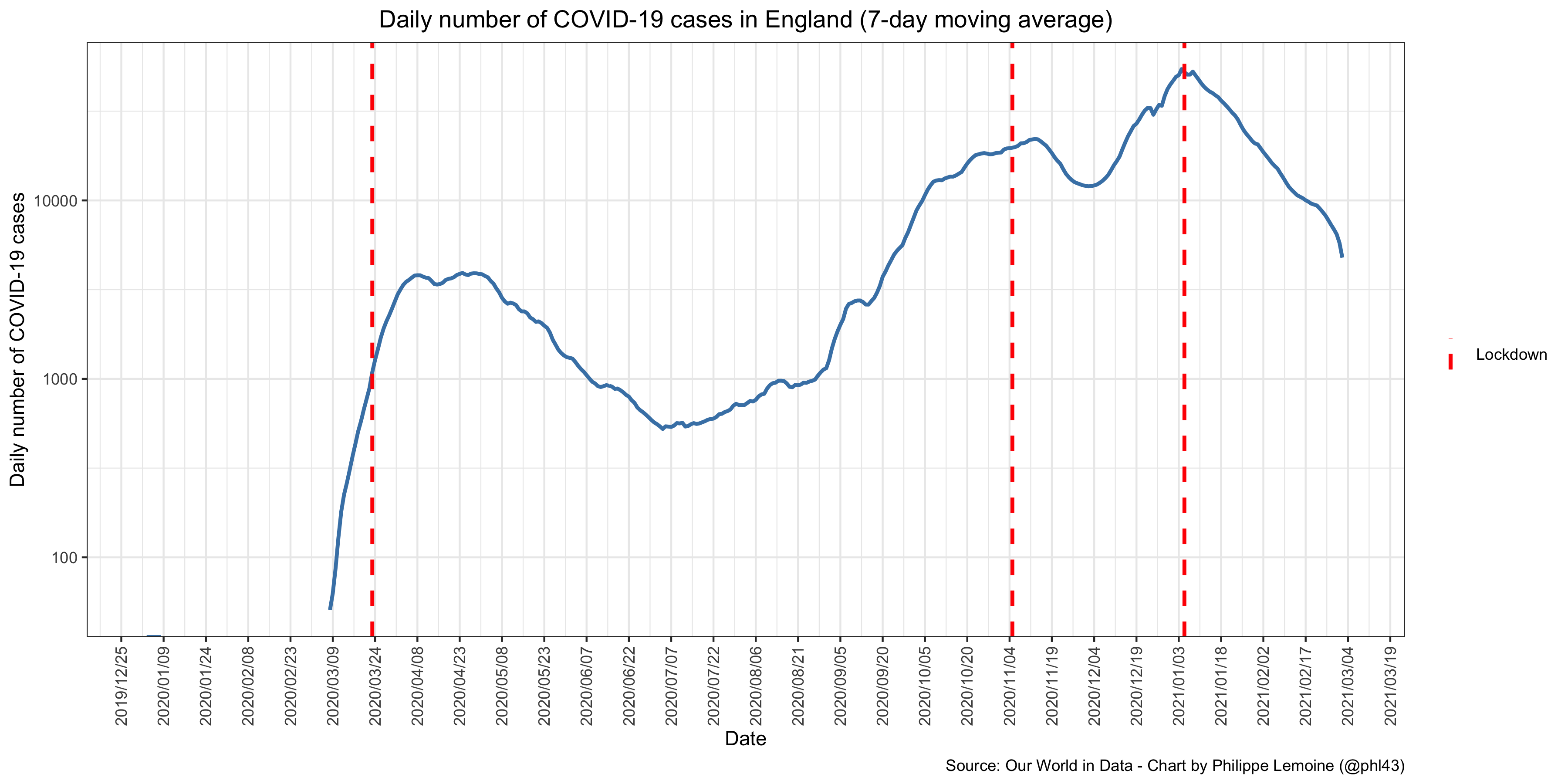 I have put the daily number of COVID-19 cases in log scale, so you can visualize the growth rate more easily. As you can see, incidence has actually been falling more rapidly after the third national lockdown than after the first, yet it wasn’t stricter and it’s doubtful that after almost a year of restrictions compliance with the rules was higher and that people’s voluntary behavioral changes were larger than during the first wave.
I have put the daily number of COVID-19 cases in log scale, so you can visualize the growth rate more easily. As you can see, incidence has actually been falling more rapidly after the third national lockdown than after the first, yet it wasn’t stricter and it’s doubtful that after almost a year of restrictions compliance with the rules was higher and that people’s voluntary behavioral changes were larger than during the first wave.
Indeed, if you look at mobility data, it’s clear that mobility fell dramatically more during the first national lockdown than during the third: Now, I know that data on cases were pretty bad everywhere during the first wave and as I already noted mobility data are probably a very noisy measure of the behaviors that drive transmission, but still you’d have to be crazy to look at these curves and conclude that it’s plausible that B.1.1.7 is 50% more transmissible than the wild type.
Now, I know that data on cases were pretty bad everywhere during the first wave and as I already noted mobility data are probably a very noisy measure of the behaviors that drive transmission, but still you’d have to be crazy to look at these curves and conclude that it’s plausible that B.1.1.7 is 50% more transmissible than the wild type.
I’m only showing the data for the UK, but to be clear, they show exactly the same thing for Ireland, Denmark and Portugal. It’s true they have all locked down recently, but since mobility didn’t fall as much as during the first wave and we know that it’s possible to deal with the wild type without a lockdown or even other stringent restrictions, I don’t see why it wouldn’t be possible to do the same with B.1.1.7. In fact, it looks as though B.1.1.7 will soon be dominant in many places that haven’t locked down and I predict that, even if incidence starts increasing again, it will eventually fall long before the herd immunity threshold is reached even if they persist in not locking down. Of course, part of the explanation is probably the fact that nobody was immune at the beginning of the first wave, whereas now the prevalence of immunity is pretty high in most places. But it would make no sense to ignore this fact, because it means that even if the variants really are more transmissible than the wild type, which they probably are to some extent, this will be alleviated by the fact that the prevalence of immunity is also higher, which lowers the effective reproduction number other things being equal. What all of this suggests is that, no matter how much more transmissible the variants of concern are relative to the wild type, they are not so much more transmissible that voluntary behavioral changes will not be able to prevent incidence from exploding until the herd immunity threshold is quickly reached. It follows that, by the same argument as before, lockdowns and other stringent restrictions would not pass a cost-benefit analysis, because it wouldn’t save enough people even if the lockdown were as short as the proponents of the “zero COVID” strategy claim it would be, which as I argued it almost certainly wouldn’t be.
The third argument in favor of that strategy frankly strikes me as completely ludicrous, which is why I kept it for last, but I will nevertheless try to make as strong a case for it as I can. In a nutshell, the argument is that, the more SARS-CoV-2 circulates, the higher the probability that a new variant that can evade currently existing immunity — whether induced by natural infection or vaccination — will emerge and take us back to square one, so we should again bring incidence back to a low enough level with a lockdown and then keep it there with contact tracing to make sure the population of SARS-CoV-2 remains small and minimize the probability that such a dangerous variant emerges. Some people who make that argument seem to suggest that we should aim at eradicating the virus globally to prevent that, but even if this eventually happens (which I seriously doubt if only because I don’t think it will be worth the trouble once enough people have been vaccinated), it will take years in the best case scenario and we obviously aren’t going to keep borders closed, lock down whole cities as soon as a few cases are detected and engage in very intrusive contact tracing for years. The virus will continue to circulate a lot in many areas of the world even if Europe and the US manage to suppress it durably within their borders and, if new variants that are able to evade immunity induced by current vaccines or natural infection by older variants of the virus are to emerge, they will emerge over there anyway and will reach Europe and the US as soon as they open their borders again. So I think a stronger version of the argument is that European countries and the US ought to suppress the virus within their borders and remain closed to parts of the world in which it’s still circulating a lot until almost everyone has been vaccinated and we have developed the production capacity and the infrastructure we need to quickly produce and distribute updated versions of the vaccine against hypothetical new variants of that sort.
This argument has the same problems as the others, but it’s even less plausible because it also has other, even more serious problems. Like the other arguments used to support the “zero COVID” strategy, it assumes that a lockdown would have a large enough effect on transmission relative to letting people’s voluntary behavioral changes drive incidence down to justify its cost, that contact tracing would actually be able to keep it there once it has reached a low enough level, that European countries and US states would be able to solve the coordination problem this strategy poses, etc. But while the other arguments in favor of that strategy were at least premised on actual threats, this argument says that we should try to pull off this strategy, which again has a very low probability of working and would have a very large cost even if by chance it turned out to work, as prophylaxis against variants that as far as we know don’t even exist yet and for all we know may never exist. Indeed, according to the best evidence we have, immunity induced by current vaccines or natural infection by older variants of the virus will probably work against the variants of concern that we currently know about. At least, experts seem pretty confident that it will at least protect against severe forms of the disease in the vast majority of cases, which is what really matters. Again, I think most restrictions are not justified at this point, but to the extent they are, it’s because of severe disease. Once the virus no longer causes severe illness, it will be even less sensible to have restrictions in place than it already is.
It’s true that neutralizing antibodies induced by current vaccines or natural infection by older variants seem to be less effective against B1.351, though not against B.1.1.7, but neutralizing antibodies are just one part of the immune response against SARS-CoV-2 and it seems that both natural infection by the wild type and Moderna and Pfizer’s vaccines elicit a strong T-cell response against B.1.1.7, B1.351 and P.1. (This had already been shown by another study for immunity induced by natural infection and Pfizer’s vaccine against B.1.1.7 and B1.351.) This suggests that immunity induced by current vaccines and natural infection by older variants will at least protect against severe forms of the disease. People started to panic after a study found that AstraZeneca’s vaccine had very low efficacy against B1.351, but the confidence interval is so wide that the point estimate is essentially meaningless. Again, the results I mentioned previously suggest that current vaccines and natural infection by older variants will at least protect against severe forms of the disease upon contact with B1.351, which is also what preliminary data from the trial of Johnson and Johnson’s vaccine in South Africa suggest. Indeed, while the trial found that efficacy was lower in South Africa than in the US or Latin America, the effect was moderate since efficacy against moderate to severe disease was estimated to be 57% in South Africa against 66% in Latin America and 72% in the US. Moreover, according to data released by the FDA, the difference is not even statistically significant. In any case, according to Johnson and Johnson, efficacy is 85% against severe disease across regions, which suggests that vaccines will be able to prevent hospitalization and death against not only B1.351 but also P.1. Moreover, the evidence so far doesn’t suggest that either B1.351 or P.1 is intrinsically more transmissible than the wild type, so we have no reason to think they will spread like B1.1.7, against which current vaccines seem to be very effective.
So despite all the scaremongering about variants, everything indicates that once at-risk people are vaccinated, SARS-CoV-2 will no longer cause severe illness except rarely. Eventually, new variants may emerge that evade even T-cell response induced by current vaccines and infection by older variants, but there is no reason to think it will happen before we have the capacity to quickly update the vaccines and distribute them to a large share of the population. Pfizer and Moderna have already said they had started to work on boosters to strengthen immunity against B1.351. Thus, we should continue to monitor new variants of SARS-CoV-2 closely and make the necessary investments to build this capacity, but it’s completely insane to embark on a probably futile and undoubtedly extremely costly effort to eradicate the virus in Europe or the US as prophylaxis against merely hypothetical threats. It seems that, with that line of reasoning, you could argue that we should remain locked down indefinitely to minimize the risk that a dangerous variant of one of the more than 200 other respiratory viruses currently in circulation will emerge. Of course, they’ve been around for a much longer time so they’ve had more time to explore the evolutionary landscape and they don’t individually circulate as much as SARS-CoV-2 because human populations are no longer immunologically naive to them and they have become endemic a long time ago, but again there are more than 200 of them so I don’t see how you can say that the risk is not at least as high. This fact alone, on top of everything else, should be a reductio of that argument in favor of the “zero COVID” strategy.
Conclusion
A lot of people seem to overestimate the impact of lockdowns and other stringent restrictions. Again, I’m not saying they have no effect, but the effect doesn’t seem to be as dramatic as many people claim and, in particular, it’s simply not the case that, unless a country lock down when incidence starts increasing, it will continue to increase exponentially until the herd immunity threshold is quickly reached. As I have argued, it seems that people voluntarily change their behavior so as to prevent that long before that point is reached, even in the absence of stringent restrictions. Meanwhile, lockdowns and other stringent restrictions seem to be very blunt instruments, which have a hard time targeting the behaviors that affect transmission the most. This is probably why they don’t seem to work very well as long as incidence is low and people are not scared, which in turn explains why often doesn’t immediately fall after a lockdown and why it climbs back up even while the restrictions are still in place when incidence has fallen to a low enough level. It’s true that many studies have found that restrictions have had a very large effect, but as I have explained, they are not credible in view of what descriptive statistics show and because their methods are generally unreliable, sometimes laughably so.
Not only do pro-lockdown advocates dramatically overestimate the effect of restrictions, but they seem to care about health outcomes to the exclusion of almost everything else. In particular, they are overly concerned about the threat of overwhelming hospitals, while not caring enough about the costs that restrictions impose on the population. Of course, it’s bad to overwhelm hospitals, but so is depriving kids of a normal childhood by preventing them from attending school in-person or socializing with their friends, closing small businesses that may keep productivity low but have large positive externalities for local communities, impoverishing students and ruining their mental health because the kind of businesses where they traditionally find jobs to support themselves have been forced to close and they aren’t able to socialize anymore, etc. When you point out those kinds of consequences, pro-lockdown advocates are quick to retort that governments could do a better job at alleviating them and in many cases they are even right, but the reality is that political constraints can’t be wished away and they often prevent that.
As I have argued above, even when you make preposterous assumptions, lockdowns and other stringent restrictions don’t pass a cost-benefit test even right now when relatively few at-risk people have been vaccinated, so this is only going to become more true as the vaccine rollout continues and picks up the pace. Even a quick and dirty cost-benefit analysis is enough to convince oneself that the costs of stringent restrictions outweigh their benefits by such a huge margin that only collective hysteria can explain why so many people continue to support those absurd policies. Not only would societies as a whole be much closer to the optimum from a cost-benefit perspective if we immediately started to lift stringent restrictions, but many people individually could improve their well-being by not refraining from certain activities that don’t seem to have a large impact on transmission, which they don’t realize because of all the scaremongering. Unfortunately, not only are pro-lockdown advocates not learning from our past experience, but many of them are doubling down with the so-called “zero COVID” policy, which is even more ridiculous from a cost-benefit perspective than less radical pro-lockdown stances. The proponents of that strategy clearly haven’t considered the costs their policy would have, the obstacles it would face and the benefits it would bring compared to more liberal policies. If they had, they wouldn’t suggest that we embark on such a project to address threats we actually face, let alone hypothetical threats such as variants capable of completely evading currently existing immunity.
Even though many governments around the world have been abolishing many of the individual freedoms traditionally enjoyed by their populations for months, as far as I know, not a single one of them has published a cost-benefit analysis to justify this policy, even though it’s something they routinely have to do in order to make far less consequential decisions. Even if you think that restrictions are justified, this should be very concerning to you and you should be clamoring for such a cost-benefit analysis to be published. I don’t think I’m being unreasonable when I say that, if governments need to publish a cost-benefit analysis before they build a bridge, they should also have to publish one before they abolish the basic freedoms of millions of people for months. I can understand why this wasn’t possible during the first wave, when everyone was taken by surprise (which incidentally was already a huge failure, but that’s another story), but now they’ve had months to do it and it doesn’t seem to have even occurred to them. Many governments have committed the most radical violations of human rights in the West since the end of WW2, not because doing so is justified by sound epidemiological and moral reasoning, but rather because they are playing it by ear and have fallen prey to the hysteria that has taken over both the media and the experts that advise them. Indeed, let’s not forget about the role played by parts of the scientific community in that debacle, which have been fueling the hysteria in question with studies that sometimes are so bad they come very close to scientific fraud. I’m convinced that eventually it will be widely acknowledged that we overreacted, but a lot of damage has already been done and I fear that, by the time enough people wake up, even more will have been done.
from Hacker News https://ift.tt/2MKVR5q

No comments:
Post a Comment
Note: Only a member of this blog may post a comment.