It was a Tuesday in early November when federal agents from the Drug Enforcement Administration paid a visit to the office of Dr. David Bockoff, a chronic pain specialist in Beverly Hills. It wasn’t a Hollywood-style raid—there were no shots fired or flash-bang grenades deployed—but the agents left behind a slip of paper that, according to those close to the doctor’s patients, had consequences just as deadly as any shootout.
On Nov. 1, the DEA suspended Bockoff’s ability to prescribe controlled substances, including powerful opioids such as fentanyl. While illicit fentanyl smuggled across the border by Mexican cartels has fueled a record surge in overdoses in recent years, doctors still use the pharmaceutical version during surgeries and for soothing the most severe types of pain. But amid efforts to shut down so-called “pill mills” and other illegal operations, advocates for pain patients say the DEA has gone too far, overcorrecting to the point that people with legitimate needs are blocked from obtaining the medication they need to live without suffering.
One of Bockoff’s patients who relied on fentanyl was Danny Elliott, a 61-year-old native of Warner Robins, Georgia. In March 1991, Elliott was nearly electrocuted to death when a water pump he was using to drain a flooded basement malfunctioned, sending high-voltage shocks through his body for nearly 15 minutes until his father intervened to save his life. Elliott was never the same after the accident, which left him with debilitating, migraine-like headaches. Once a class president and basketball star in high school, he found himself spending days on end in a darkened bedroom, unable to bear sunlight or the sound of the outdoors.
“I have these sensations like my brain is loose inside my skull,” Elliott told me in 2019, when I first interviewed him for the VICE News podcast series Painkiller. “If I turn my head too quickly, left or right, it feels like my brain sloshes around. Literally my eyes burn deep into my skull. My eyes hurt so bad that it hurts to blink.”
After years of trying alternative pain treatments such as acupuncture, along with other types of opioids, around 2002 Elliott found a doctor who prescribed fentanyl, which gave him some relief. But keeping a doctor proved nearly impossible amid the ongoing federal crackdown on opioids. Bockoff, Elliott said, was his third doctor to be shut down by the DEA since 2018. As Elliott described it, each transition meant weeks or months of desperate scrambling to find a replacement, plus excruciating withdrawals due to his physical dependence on opioids, followed by the return of that burning eyeball pit of despair.
After the DEA visited Bockoff on Nov. 1, Elliott posted on Twitter: “Even though I knew this would happen at some point, I'm stunned. Now I can't get ANY pain relief as a #cpp [chronic pain patient.] So I'm officially done w/ the US HC [healthcare] system.”
Privately, Elliott and his wife Gretchen, 59, were frantically trying to find another doctor. He sent a text to his brother, Jim Elliott, saying he was “praying for help but not expecting it.”
Jim, a former city attorney for Warner Robins who is now in private practice, was traveling when he received his brother’s message. They made plans to talk later in the week, after Danny had visited a local physician for a consultation. In subsequent messages, Danny told Jim that Gretchen had reached out to more than a dozen doctors. Each one had responded saying they would not take him as a patient.
Jim recalled sensing in Danny “a level of desperation I hadn't seen before.” Then, on the morning of Nov. 8, he woke up to find what he called “a suicide email” from his brother. Jim called the local police department in Warner Robins to request a welfare check. The officers arrived a few minutes before 8:30 a.m. to find both Danny and Gretchen dead inside their home.
A police report obtained by VICE News lists a handgun as the only weapon found at the scene. Warner Robins police said additional records could not be released because the case is “still active.” The department issued a press release calling the deaths a “dual suicide.”
Jim shared a portion of a note that Danny left behind: “I just can't live with this severe pain anymore, and I don't have any options left,” he wrote. “There are millions of chronic pain patients suffering just like me because of the DEA. Nobody cares. I haven't lived without some sort of pain and pain relief meds since 1998, and I considered suicide back then. My wife called 17 doctors this past week looking for some kind of help. The only doctor who agreed to see me refused to help in any way. What am I supposed to do?”
At a joint funeral for Danny and Gretchen Elliott on Nov. 14 in Warner Robins, mourners filled a mortuary chapel to overflow capacity. Eulogies recalled a couple completely devoted to each other. They were doting cat owners, dedicated fans of Georgia Tech and Atlanta sports teams, and devout Christians, even as Danny’s chronic pain increasingly left him unable to attend church. In photos, the Elliotts radiate happiness with their smiles. But their lives were marred by pain: Gretchen was a breast cancer survivor. She married Danny in 1996, well after his accident, signing up to be his caregiver as part of their life partnership.
“It was a Romeo and Juliet story. They didn't want to live without each other,” said Chuck Shaheen, Danny’s friend since childhood and Warner Robins’ former mayor. “I understand the DEA and other law enforcement, they investigate and then act. But what do they do with the patients that are no longer able to have treatment?”
Shaheen and Danny both worked in years past for Johnson & Johnson, which is among the companies sued for allegedly causing the opioid crisis. Shaheen was also previously a salesperson for Purdue Pharma, the maker of OxyContin, another company blamed for spreading addiction. But Shaheen said Danny was not among those chasing a high—he, like others with severe chronic pain, was just seeking a semblance of normalcy.
“They're not doctor shopping,” Shaheen said. “They're not trying to escalate their dose. They're trying to function.”
Danny told me in 2019 that the relief he obtained from fentanyl didn’t make him feel euphoric or even completely pain free. He was using fentanyl patches and lozenges designed for people with terminal cancer pain, at extremely high doses that raised eyebrows whenever he was forced to switch doctors. But it was the only thing that worked for him.
“I call it turning the volume of my pain down from an eight or nine or even 10 sometimes to a six or a five,” he said. “The pain doesn't get much lower than that, but for me, that's almost pain free. It was the happiest thing I've ever experienced in my life.”
There are millions of chronic pain patients suffering just like me because of the DEA. Nobody cares
Gretchen’s brother, Eric Welde, choked up as he spoke with VICE News at the funeral about his perspective on the family’s loss: “In my mind, what the DEA is essentially doing is telling a diabetic who's been on insulin for 20 years that they no longer need insulin and they should be cured. They just don't understand what chronic pain is.”
So far, no criminal charges have been filed against Bockoff. In response to an inquiry from VICE News about the deaths of Danny and Gretchen Elliott, the doctor emailed a statement that said: “I am unable to participate in an interview except to say: Their blood is on the DEA’s hands.”
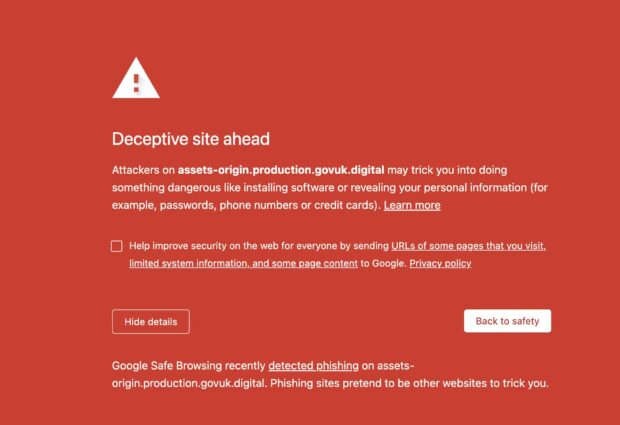
The DEA responded to a list of questions about Bockoff and the Elliotts’ suicides with an email saying Bockoff received what’s known as an “Immediate Suspension Order,” which according to public records is warranted in cases where the agency believes the prescriber poses “an imminent danger to public health or safety.” The DEA said local public health partners were notified in advance to coordinate under a federal program designed to mitigate overdose risks among patients who lose access to doctors. The agency offered no further comment.
Data on suicides by chronic pain patients is scarce, but experts who study these cases estimate that hundreds—perhaps thousands—of Americans have taken their own lives in the aftermath of losing access to prescription opioids and other medications. Some cases have occasionally made news, like a woman in Tennessee who was arrested for buying a gun to assist her husband’s suicide after his doctor abruptly cut down on his medication used to treat back pain.
Starting around 2016, a backlash to prescribing opioids began to spread across the U.S. healthcare system, sparked in part by guidance from the Centers for Disease Control and Prevention (CDC) that prompted scrutiny of patients on doses equivalent to over 90 milligrams of morphine per day.
The National Committee for Quality Assurance, which develops quality metrics for the healthcare industry, has implemented its own 90 milligram threshold, and patients over that baseline count as receiving “poor care,” regardless of their dose history. In practice that means doctors have strong incentives to reduce the dosage, even for someone like Elliott, who had been taking the same prescription for years, and even if it’s not necessarily in the best interests of the patient.
Since 2018, the CDC has developed an initiative called the Opioid Rapid Response Program, which is supposed to assist when doctors lose the ability to prescribe pain medication. Stephanie Rubel, a health scientist in CDC’s Injury Center who leads the program, said when the DEA visited Bockoff’s office, “a healthcare professional was onsite in case any patients arrived for their appointments.”
Rubel, in a statement sent via the CDC’s press office, said everyone from the county health department to Medicare providers were alerted about the DEA’s action against Bockoff. But Rubel also noted that the CDC program “does not provide direct assistance to patients affected by a disruption, including referrals or medical care.” In fact, the only help that patients like Elliott received was a flier with a list of local emergency rooms they could visit if—or when—they started experiencing withdrawal.
“Any loss of life due to suicide is one too many,” Rubel said. “This case is heartbreaking and emblematic of the trauma, pain and danger many patients face when these disruptions occur and is why ORRP [Opioid Rapid Resposne Program] has been developed to help prepare state and local jurisdictions to respond when disruptions in care occur.”
Dr. Stefan Kertesz, a professor at the University of Alabama at Birmingham Heersink School of Medicine, had been acquainted with Danny since 2018, meeting him in another moment of crisis. Danny’s doctor at the time had just been arrested by the DEA, and Kertesz, who conducts research and advocates on behalf of chronic pain patients, stepped in to help. It was difficult, Kertesz told VICE News, because “the doses he was on were orders of magnitude higher than most doctors are familiar with.”
What the DEA is essentially doing is telling a diabetic who's been on insulin for 20 years that they no longer need insulin and they should be cured
Danny ultimately found another doctor but was forced to change once more before landing with Bockoff in Beverly Hills. Kertesz cautioned that he was not familiar with the details of Bockoff’s case, but said the doctor was known for treating “opioid refugees” who’d been turned away from other physicians. Danny and his wife would fly from Georgia to Los Angeles for appointments, and other patients with unique circumstances came from around the country.
Bockoff had practiced medicine in California for 53 years with no record of disciplinary action or complaints with the state medical board, according to the Pain News Network, which reported the DEA searched the doctor’s office about a year ago. The DEA took, but eventually returned, some patient records.
Asked about the DEA’s handling of the Bockoff case, Kertesz replied: “Honestly, it seemed to me like bombing a village. It could be they think they're getting the bad guy, but it's not a precision munition. Whoever is launching the bomb has to consider the collateral damage.”
Clinical research on chronic pain patients is complicated, Kertesz said, but “a lengthy series of studies confirm that there is a strong association between opioid reduction or stoppage and suicide.” While reducing opioid intake can be helpful for some people, he said, Danny and other longtime users with medical needs should not be forced to go cold turkey.
“Even if you believe the doctors did something wrong, I can't find somebody who believes all those patients should die,” Kertesz said. “And if we agree they shouldn't all die, then why would we act in such a way that we know we're going to massively increase their risk of death?”
Another former Bockoff patient was Kristen Ogden’s husband Louis. Much like Gretchen Elliott, Ogden has supported her husband for years as he’s battled chronic pain caused by a rare condition similar to fibromyalgia. And like the Elliotts, the Odgens have dealt with the fallout of DEA actions that triggered desperate searches for new doctors.
The Ogdens live in Virginia and had just landed in California for a doctor’s appointment when they got the news about the DEA’s visit to Bockoff’s office. They found the emergency room flier to be a slap in the face.
“They probably look at you as an addict and they recommend that you do whatever you can to get off these medications,” Ogden said. “They're not there to help us at all.”
Ogden is the co-founder of an advocacy group called Families for Intractable Pain Relief, and she started reaching out to her network, including other patients. She spoke to Danny by phone and described him as sounding “consumed by this dread of what he fully expected was going to be the next step for his life—months of untreated pain.”
Honestly, it seemed to me like bombing a village
Ogden said she’s personally called at least 10 doctors seeking treatment for her husband but to no avail. Other Bockoff patients are in the same boat, she said, and nobody she knows has been able to find another specialist willing to continue with a similar course of care.
Dr. Thomas Sachy of Gray, Georgia, was the first doctor to prescribe Danny fentanyl and remained his physician until the DEA raided his practice in 2018. Federal authorities have alleged Sachy had his office set up like a “trap house” with firearms on the premises. Sachy is charged with “issuing prescriptions not for a legitimate medical purpose and not in the usual course of professional practice.” Two employees and Sachy’s 84-year-old mother, who worked at his clinic, were also initially charged but their cases have since been dropped.
Sachy agreed to plead guilty in the case to avoid a possible life sentence but later withdrew the plea. He maintains his innocence. His trial is scheduled to start in January in federal court in Georgia. Wearing an electronic ankle monitor to track his location while out on bond, Sachy attended the Elliotts’ funeral service in Warner Robins, where he sat for an interview with VICE News.
Federal prosecutors have accused Sachy of prescribing opioids that contributed to the deaths of patients. Sachy in turn blames the DEA for the suicides of two patients who took their lives in the aftermath of the raid.
“My patients weren't young drug addicts off the street,” Sachy said. “They were middle-aged and older with health problems. And the thing about pain, chronic pain, and the anxiety and the suffering that comes with it, it wears you down.”
Similar to what happened with Bockoff, after the DEA visited Sachy’s office in Georgia, the only resource made available to patients was a list of local pain management facilities and resources for opioid withdrawal, including emergency rooms. Sachy scoffed at the idea of his patients visiting an ER for help: “They'd look at them like they were insane or criminals or both.”
“It's absolutely frustrating,” Sachy said. “It's absolutely heartbreaking. It sucks. It destroys everything you think a physician should do and be and should be able to accomplish. It’s all taken away. And it's just utter helplessness.”
Among the Elliott family and other pain patients, helplessness and anger remain common sentiments. Ogden said her husband and other chronic pain patients have spoken with an attorney about the possibility of a lawsuit against the DEA.
As a lawyer who worked for years in public office, Jim Elliott knows civil litigation against the government can be an uphill battle. He said the family is still deciding how to move forward in response to the deaths of Danny and Gretchen.
Jim emphasized that “it wasn't as if pain medication made Danny's life great.”
Fentanyl just made the pain bearable. And when that was taken away, Danny saw no future.
“He was taking a high level of pain medication but he wasn't an addict and he wasn't trying to get high or anything,” Jim Elliott said. “He was just trying to live a life. And they closed every door for people like that.”
If you are in crisis, please call the National Suicide Prevention Lifeline at 1-800-273-TALK (8255), or contact the Crisis Text Line by texting TALK to 741741.